Osteoarthritis is common problem causing joint disease. The cause of osteoarthritis is complicated, but increases in inflammatory enzymes and cytokines have been correlated with joint damage in early osteoarthritis (He et al, 2020; Attur et al, 2015). These inflammatory markers have become a target of potential therapies.
Alpha-2-macroglobulin (A2M), a naturally occurring molecule that is found in the blood serum. Previous studies have demonstrated A2M can bind to and neutralized these destructive catabolic enzymes (Crookston et al, 1994; Feige et al, 1996; Dzhugashvili et al, 2014; Demirag et al, 2004; Demirag et al, 2005). By neutralizing these destructive enzymes, it is thought that A2M may affect the breakdown of cartilage (LaMarre et al, 1991; Santos et al, 2016).
The overall mechanism of how A2M works remains unclear. In osteoarthritis, various inflammatory enzymes and cytokines have been correlated with joint damage after a joint injury (Attur et al, 2015; Anderson et al, 2011; Backus et al, 2011; Borrelli et al, 2003; Tochigi et al, 2011).
A2M is thought to inhibit the majority of these destructive catabolic enzymes and cytokines that cause inflammation and degrade cartilage (Claassen et al, 2011; Wang et al, 2014). In vitro and pre-clinical studies have demonstrated that by neutralizing these destructive enzymes, A2M has a broad ability to block catabolic cytokines and enzymes (Wollenberg et al, 1991; Borth et al, 1990) and may reduce catabolism‐associated cartilage damage (Wang et al, 2014; Mathew et al, 2015; Wang et al, 2014; Zhang et al, 2017).
Osteoarthritis is a common disease with a complex. Current treatment options mainly provide symptom relief, but generally do not halt the progression of osteoarthritis to severe joint degeneration.
A2M has emerged as a potential procedure that may able to slow the development of early cartilage damage in in vitro and pre-clinical studies. A2M has strong anti-inflammatory effects, and is a broad spectrum inhibitor of several chemicals that slowly erode cartilage and neutralizes their degenerative effect, but few clinical studies have assessed the use of A2M in human subjects.
A2M injections are not the same as a platelet-rich plasma or PRP injection. In traditional PRP injections the A2M molecules are not concentrated.
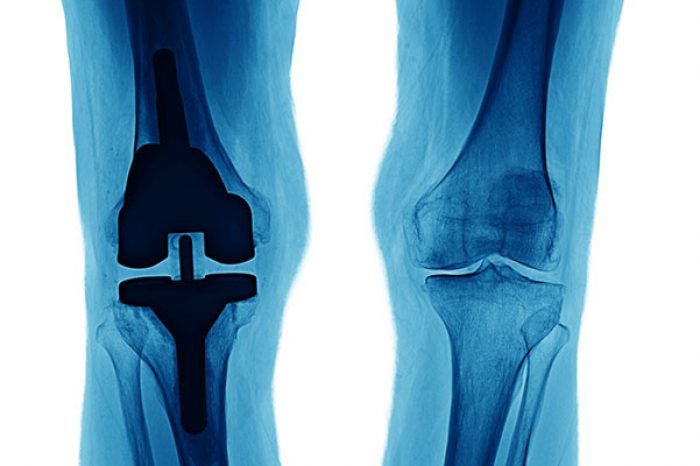
In an A2M injection, the A2M proteins are concentrated. At your appointment, your blood will be drawn and spun in a centrifuge similar to a traditional PRP injection. For an A2M injection, an additional step is performed using a special device to filter the plasma and concentrate the A2M macromolecules. Once the concentrated, the solution of A2M can then be injected into the arthritic joint.
Osteoarthritis is a common disease. Current treatment options mainly provide symptom relief, but generally do not halt the progression of osteoarthritis. A2M has emerged as an orthobiologic procedure for osteoarthritis, and theoretically has been discussed by Sun et al as potentially being able to slow or halt the development of early cartilage damage into significant disease (Sun et al, 2023).
There is limited clinical data to guide patient selection and few studies have compared the use of A2M to other injectable treatments in osteoarthritis.
Alpha-2-macroglobulin (A2M) is a naturally occurring macromolecule, but little clinical data exists on the use of injectable macromolecules for the management of osteoarthritis of the knee.
In one prospective randomized controlled trial performed at NYU, 75 patients were divided into 3 groups and given either a PRP, A2M or corticosteroid injection. Patients were followed for 12-weeks. At the final follow-up visit at 12-weeks after the injection, the A2M group had a statistically significant improvement in functional scores compared to the PRP and corticosteroid groups(-18.4 v -5.7 v -7.1, p =0.03), and the study demonstrates Alpha-2-Macroglobulin decreased arthritic symptoms more than traditional PRP and corticosteroid injections (Klein et al, 2020). The major limitation of this study is that it provided no long term data on how patients did after that final follow-up visit at 12-weeks.
Meniscus tears are one of the most common causes of knee pain in active adults and aging athletes alike. If you’ve been told you have a “degenerative meniscus tear,” you may have also heard that surgery isn’t always the
Read MoreFor patients with chronic adductor longus tendinopathy, a newer option is emerging: ultrasound-guided tenotomy using the Tenex system. Recent clinical evidence suggests this minimally invasive approach may effectively
Read More