Dupuytren’s disease is a hand deformity that takes years to advance and often begins with nodules and bands, that are sometimes painful. Often mistakenly diagnosed as arthritis or tendinitis, the current treatment options are limited and have a high rate of recurrence. Recent studies suggest that extracopreal shockwave therapy can be effective in decreasing pain and slowing the progression of Dupuytren’s disease.
What is Dupuytren's disease?
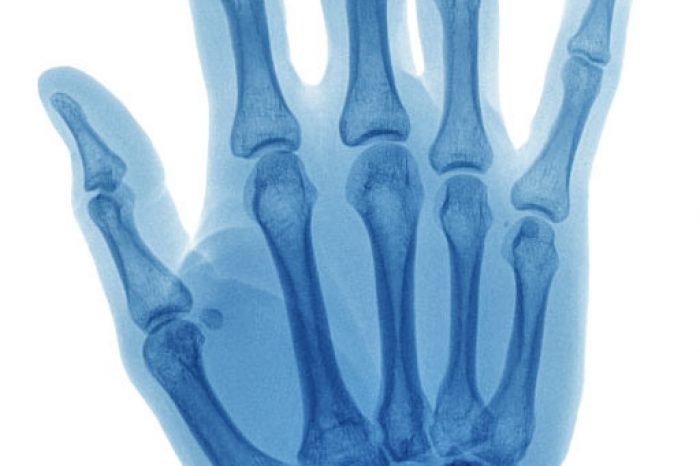
Dupuytren's disease is a progressive disease due to thickening of the fibrous tissue in the palm. Often, people with Dupuytren’s contracture mistakenly assume they have arthritis or tendinitis, or don’t notice a problem until their fingers start to bend.
As the disease progresses, fibrous cords and nodules form in the palmar fascia and patients develop pain and a loss of motion affecting the fingers. At a later stage in the disease process, patients may lose the ability to hold objects.
Who is at risk of Dupuytren's disease?
Dupuytren's disease commonly affects male over 50 years of age. Various risk factors have been associated with Dupuytren's disease and certain genetic factors may predispose patients to Dupuytren's disease.
How is Dupuytren's disease diagnosed?
The diagnosis is usually clinical and based on signs and symptoms.
How is Dupuytren's disease traditionally treated?
Surgery is often the main treatment option provided to patients (Balaguer et al, 2009), and excision of the affected tissue and correction of any finger contractures is considered the gold standard. Alternative non-surgical treatments are available and include enzymatic fasciotomy with collagenase injections (Xiaflex)(Peimer et al, 2015), needle aponeurotomy (Scherman et al, 2018), and radiotherapy (Keilholz et al, 1996).
One limitation of these current treatment options is the rate of recurrence. Dupuytren’s is a scarring condition, and surgery can be a scarring procedure so there can be failure. In a systematic review by Werker et al., the rate of recurrence was found between 12% and 100% following surgeries performed at different stages of the disease (Welker et al, 2012). In another systematic review by Chen et al.,[12] the rate of recurrence was 12%–39% following open partial fasciectomy (at a 1.5–7.3 years follow up), 50%–58% following needle aponeurotomy (at 3–5 years follow up), and 10%–31% after collagenase injections (at the 3 months to 4 years follow up) (Chen et al, 2011).
How does shockwave treatments work for Dupuytren's disease?
Extracorporeal shock wave therapy (ESWT) is an effective and safe non-invasive treatment for many orthopedics diseases (Schmitz et al, 2015). Shock waves are not electrical shocks, but pressure waves generated through various mechanisms. Radial ESWT (rESWT), compared with conventional focused ESWT, is a low- to medium-energy shock wave and designed to provide the maximum energy at the probe tip and distribute it radially into the tissue.
Considering that Dupuytren's disease contractures are superficial, it has been hypothesized that radial extracorporeal shock wave therapy could be an effective treatment to reduce contractures and improve hand function (Brunelli et al., 2020). Radial ESWT has broader and safer effect than focused shock wave therapy which targets deeper tissue and often is more expensive (Ramon et al, 2015).
Although shock wave therapy is FDA-approved for treating other musculoskeletal conditions, it is still an “off-label” remedy for Dupuytren’s and is still not widely in use for treating the condition.
What is the evidence for shockwave treatments for Dupuytren's disease?
In a recent case report published by Brunelli et al. (2020), a 79-year-old gentleman with a 4-year history of impaired left-hand function and diagnosed with Dupuytren's disease impacting the ring and middle finger was treated with 4 weekly sessions of radial extracorporeal shock wave therapy. There was temporary worsening of symptomatology for a day after the first few sessions, but after the 4th treatment there was a reduction of nodule and cord dimensions. The contracture also reduced by 15 degrees.
Another case report by Taheri et al. (2021) described a 64-year-old farmer with Dupuytren’s disease in both hands with flexion contracture of the 4th finger. The patient was treated with 6 weekly radial shock wave treatments. The patient had improved range of motion and better hand function after the treatment.
In another case series of 23 patients, patients demonstrated improved pain and function with significant improvement in grip strength. Patients had 6 weekly treatments with the Roland Electronica Pagani SRL device (Aykut et al, 2018).
In a randomized controlled study, Notarnicola et al (2017) compared shockwave and high-energy laser therapy to stretching exercises in 45 patients with Dupuytren’s disease. Shockwave was the only treatment that demonstrated improved function at all follow up intervals and after the final treatment patient satisfaction was highest for shockwave treatments (Notarnicola et al, 2017).
Conclusion
Extracorporeal shock wave therapy (ESWT) is an effective and safe non-invasive treatment for many orthopedics diseases, but is still not widely in use for treating Dupuytren’s disease. Early studies suggest that shock wave therapy appear safe, and has good efficacy with good patient satisfaction for treating Dupuytren’s diseasetofor treating Dupuytren’s disease.
References
Is stem cell therapy better than cortisone for knee arthritis? Learn the differences, risks, benefits, and long-term results of cortisone vs stem cell knee injections.
Read More