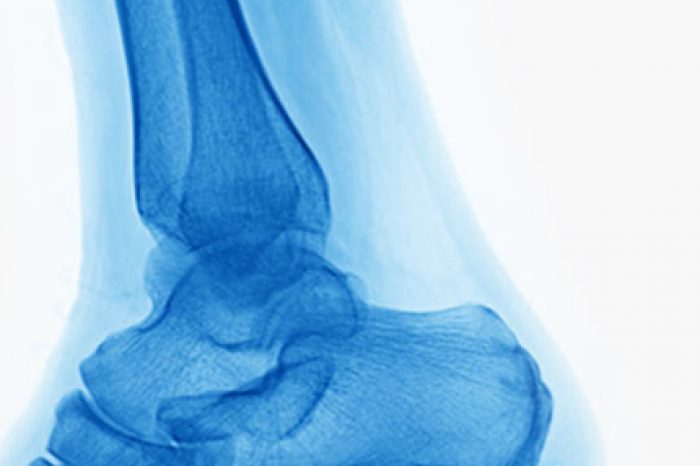
Plantar fasciitis is the most common cause of heel pain, affecting millions of people worldwide [Orchard, 2012]. It happens when the thick tissue on the bottom of the foot, called the plantar fascia, becomes damaged due to overuse or strain. For years, treatments like physical therapy, shoe inserts, and medications have been the standard of care. For patients who do not respond to these interventions interventions, different types of injections are available.
The current standard for local injection therapies includes
corticosteroid injections, however, many patients only experience
partial improvement and the benefits tend to diminish over time. In
recent years, platelet-rich plasma (PRP) injections have gained prominence in the treatment of plantar fasciitis by leveraging the regenerative potential of platelets and leukocytes leukocytes [Molloy et al, 2003].
The efficacy of PRP versus corticosteroid treatment for plantar fasciitis remains controversial, as various randomized controlled trials (RCTs) have yielded conflicting results. A recent systematic review and meta-analysis comparing PRP to corticosteroids hopes to clarify the confusion and help determine if one treatment is superior for managing pain and improving foot function in patients with plantar fasciitis.
The current standard for injections for plantar fasciitis includes corticosteroid injections. Corticosteroids are powerful medications used to reduce inflammation and provide short-term pain relief. They're injected directly into the affected area and work quickly, which provide short-term pain relief in approximately 70-80% of patients, but their effects tend to wear off after a few months with the pain relief generally last only between 4 to 12 weeks. The greatest relief tends to be observed around 4 weeks post-injection [Speed, 2007; McMillan et al, 2012; Whittaker et al, 2019; David et al, 2017].
PRP is a treatment made from a patient’s own blood. After being processed, the blood is rich in growth factors that help the body heal by promoting tissue repair. Unlike corticosteroids, PRP focuses on rebuilding the damaged tissue, not just relieving pain.
This study identified 24 randomized controlled trials comparing PRP and corticosteroid injections for the treatment of plantar fasciitis. The authors performed a meta-analysis and found that that, compared to corticosteroid injections, local injections of PRP provided better relief from pain and improvement in foot and ankle function at 3 to 6 months.
This Study’s Key Findings Are:
Plantar fasciitis pain is not due to inflammation, but is caused by repetitive microtrauma and excessive tension on the plantar fascia, which leads to microtears within the fascia [Thompson et al, 2014]. These microtears result in swelling, edema and degenerative changes, which cause structural damage and pain in patients with plantar fasciitis.
Corticosteroids treat inflammation, which is why they workquickly. PRP, on the other hand releases a concentrated array of growth factors, which are pivotal in tissue repair and regeneration, which takes time but leads to longer-lasting results [Hall et al, 2009].
Based on this recent systematic review and meta-analysis, PRP "is a promising therapeutic option, particularly for patients who have not responded adequately to conventional treatments treatments." PRP appears to offer better results over the long-term without the risks linked to repeated corticosteroid injections.
While both treatments can help, PRP has the ability to improve pain and function in the long term.
(781) 591-7855
20 Walnut St
Suite 14
Wellesley MA 02481
Meniscus tears are one of the most common causes of knee pain in active adults and aging athletes alike. If you’ve been told you have a “degenerative meniscus tear,” you may have also heard that surgery isn’t always the
Read MoreFor patients with chronic adductor longus tendinopathy, a newer option is emerging: ultrasound-guided tenotomy using the Tenex system. Recent clinical evidence suggests this minimally invasive approach may effectively
Read More