Frozen shoulder, or adhesive capsulitis, is a condition that causes pain and restricted movement in the shoulder. The joint of the shoulder is held together by a joint capsule, which becomes thickened and results in a global restriction of shoulder movement. This manifests with shoulder motion being stuck or frozen in all planes of motion, and loss of motion especially in external rotation is an early sign.
Frozen shoulder is a poorly understood disease. Genetic and environmental factors likely play an important role.
Anyone can get a frozen shoulder. In the general population, the incidence of frozen shoulder is 5%. In diabetics the incident can be as high as 20% (Sharma, 2011), with frozen shoulder being twice as common in insulin-dependent diabetics compared with non-insulin dependent diabetics (Yian et al., 2012). Patients with Dupuytren’s disease are also at increased risk, and are 8 times more likely to develop a frozen shoulder (Smith et al., 2001).
Various other triggers have been associated with adhesive capsulitis, including trauma, surgery (not just limited to the shoulder), stroke, thyroid disorders, and other inflammatory diseases. Periods of immobilization are also a risk factor for adhesive capsulitis (Bruckner & Nye 1981).
Frozen shoulder progresses in a predictable manner.
The diagnosis of frozen shoulder is typically made clinically, and often by the diagnosis can be made by testing the range of motion in the shoulder.
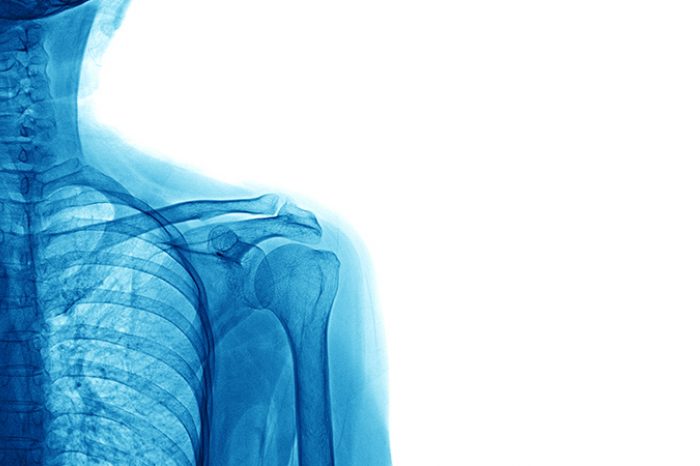
X-rays and an MRI can differentiate frozen shoulder from alternative causes of shoulder pain such as osteoarthritis, posterior shoulder dislocation, rotator cuff calcification or tumors.
Historically, patients were reassured that frozen shoulder will resolve with conservative treatment or observation. In some reports, frozen shoulder resolved in 94-96% of patients over a 2-year period or longer (Grey, 1978; Vastamaki et al. 2012).
In other reports, the rates of complete recovery were as low as 39-50% (Reeves, 1975; Shaffer et al., 1992). In one study, 40% of patients had persistent symptoms at the 3 year follow up (Hand et al 2008).
It is unusual for adhesive capsulitis to recur in the same shoulder, but in one report 14% of people develop it in the opposite shoulder (Smith et al. 2014).
The stage of the disease process influences treatment options. Often medications and early activity are the first-line treatments. Physical therapy is often prescribed and joint mobilization with a therapist has been shown to be better than stretching exercises alone (Celik & Mutlu, 2016). In the majority of patients, 60-95% respond to a combination of therapy or medications (Schoch et al. 2020).
Shoulder hydrodilation or high-volume shoulder distension is a non-surgical treatment for frozen shoulder. The treatment involves injecting a high volume of saline and local anesthetic into the glenohumeral joint under ultrasound guidance. The objective of the treatment is to physically expand or distend the joint capsule, but the exact mechanism of the procedure is debated.
One study has shown that a high-volume distention of the joint capsule combined with mobilization and a corticosteroid injection was the most effective treatment for adhesive capsulitis (Park et al. 2014). Other studies have now shown clear superiority, but technique, volume of injectate and post-procedure manipulation may account for some of the variability in the outcome of these studies (Tveita et al, 2008; Sharma et al 2016). In one study, high-volume dilation without manipulation is less effective than intensive manipulation alone suggesting that the technique and protocol used by your physician matters (Park et al. 2014).
In one study comparing surgery to high-volume distention both groups of patients had significant improvement in range of motion and there was no significant difference in pain scores (EQ-5D VAS) at any time point (Gallacher et al. 2018). While surgery did have a significant improvement in the Oxford Shoulder Score, the results were otherwise comparable between non-operative management with high-volume shoulder dilation and surgery. High-volume dilation should be considered before surgery.
Learn more about frozen shoulder and high-volume dilation.
Some studies have also explored the use of PRP for adhesive capsulitis.
Is stem cell therapy better than cortisone for knee arthritis? Learn the differences, risks, benefits, and long-term results of cortisone vs stem cell knee injections.
Read More