Tendon and ligaments are fibrous connective tissue that are prone to acute and repetitive work injuries. For example, lateral epicondylitis affects 1-3% of the general population and up to 29.3% of laborers.[1]
In cases of a partial tendon/ligament tear, tendinopathy and tendon calcification the existing medical and surgical treatments often fail to regain normal function.
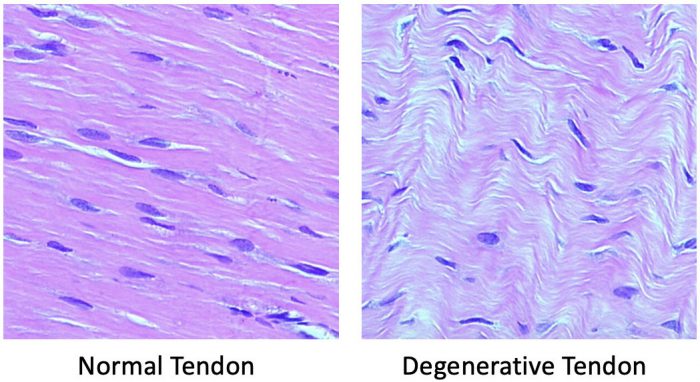
Tendons and ligament injuries heal slowly and often require lengthy periods of rehabilitation. Some patients experiencing symptoms for up to 6 to 24-months.[2, 3] In chronic cases we now know that the pain is not from inflammation,[4] but is from the normal architecture of the tendon being replaced with degenerative tissue and compromising the structural integrity of the tissue. In patients with more than 6 months of pain, they are less likely to experience spontaneous resolution of tendon pain.[5, 6]
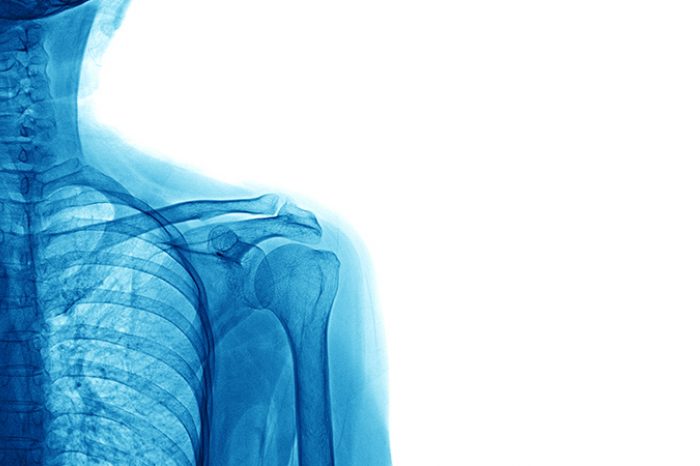
Accurate and timely diagnosis of tendon/ligament injuries ensures proper treatment and helps minimizes costs. MRI and ultrasound have both been validated against surgical and histological findings.[7] In studies comparing ultrasound to MRI for rotator cuff and Achilles tendon tears there was no statistically significant difference in sensitivity and specificity, and for smaller tendons sonography maybe more sensitive in detecting tears than MRI.[8]
Advantages of diagnostic ultrasound over MRI, include:
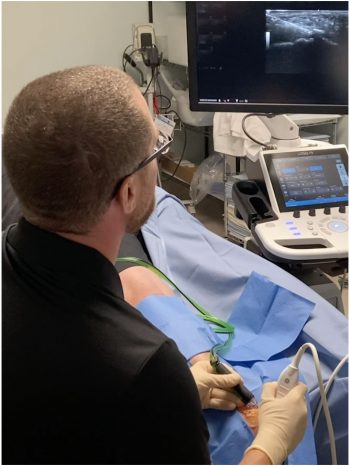
Ultrasound allows direct needle visualization as it enters the targeted tissue and UGI are more accuracy than blind injections (i.e. injections performed without imaging).[9] Even with the most experienced hands, blind injections are not 100% accurate.
Ultrasound has similar accuracy to fluoroscopically guided musculoskeletal injections with less cost, without the associated radiation and allows the physician to avoiding injuring adjacent tendon, ligaments, nerves and blood vessels.[10, 11] Ultrasound also has the distinct advantage of visualizing the soft tissue structures around the joint, making it the gold standard for tendon injections. For example, level 1 studies show blind biceps tendon injections have an accuracy of only 27% compared an accuracy of 87% with UGI.[9]
ACCURACY OF BLIND INJECTIONS
In some joints the accuracy of blind injections is as low as 30 to 40%, while in nearly every joint the accuracy of UGI exceed 90%.[9]
WHAT IS A MINIMALLY INVASIVE TRIGGER FINGER RELEASE?
More than 30% of trigger finger cases do not resolve, and these cases require a release of the A1 pully either with open surgery or ultrasound-guided release.[12, 13] Surgery requires wound care, risk of infection and a prolonged return to work due to wound healing with up to 4 weeks to be cleared to grip. Open surgeries carry a risk rate of 12 to 28%, ranging from nerve injury, vascular injury, wound infection to wound dehiscence and scar hypertrophy.[14-16]
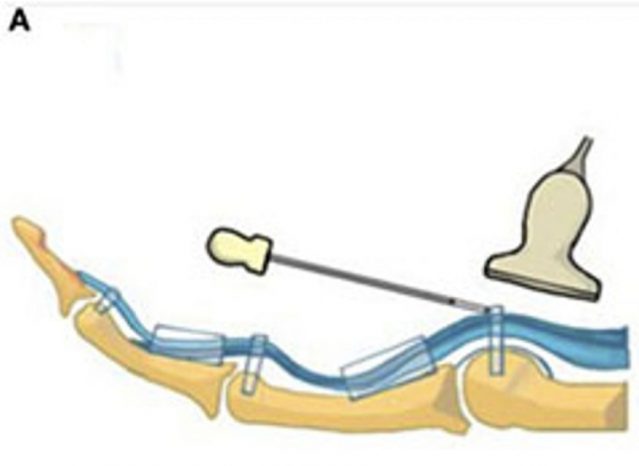
Minimally invasive trigger finger release does not require a surgical incision, is done with lidocaine locally to numb the area and release the A1 pully under ultrasound imaging. In 3 days, the patient can resume light gripping and resume full gripping in 10 days. In addition to a quicker return to work there are no surgical center costs.
Pan et al, Frontiers in Pharmacology 2019
WHAT IS PRP?
PRP is a form of regenerative medicine using a patient’s own platelets to promote healing of injured tendons, ligaments muscles and joints. PRP injections are prepared in the office by drawing a patient’s blood and concentrating the platelets before injecting into the injured or diseased tissue.
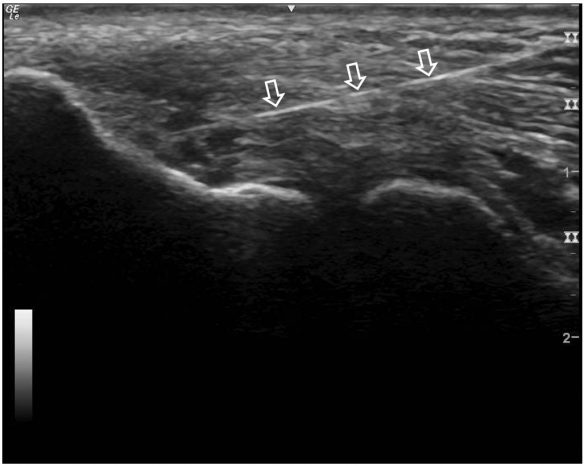
Arrows showing needle going into tendon. Dark holes in tendon represent partial tearing of the tendon.
HOW DOES PRP WORK?
When injected the concentrated platelets release growth factors to stimulate reparative cells in the body. PRP injections have been shown to stimulate collagen production and tendon cell proliferation. Moderate to high-quality evidence supports the use of PRP to enhance the healing process for lateral epicondylitis, osteoarthritis of the knee, patellar tendinopathy and plantar fasciitis.[17]
WHAT ARE THE EXPECTED RESULTS?
Ultrasound and MRI have shown tissue repair after PRP injections.[18, 19] Tissue repair occurs over weeks to months. In one study in the American Journal of Sports Medicine, patients with elbow tendinosis experienced a 60% reduction in pain by 8-weeks and 81% reduction at 6-months.[20] In another retrospective study comparing PRP to surgery for lateral epicondylitis PRP was better for pain relief and functionality in the short and mid-term, suggesting patients could return to work faster than if they had an open surgery.[21]
In a recently published study from Tulane University, outcomes with PRP were clinically similar to surgery in medial epicondylitis with an earlier return to full range of motion and pain-free status.[22] Similar outcomes in pain and return to work comparing PRP to surgery for lateral epicondylosis were noted in a study out of the University of Michigan.[23]
NOT ALL PRP IS THE SAME
Outcomes can be impacted by differences in platelet concentration, cell types and use of guidance in delivering these cells into the abnormal tendon/ligaments.
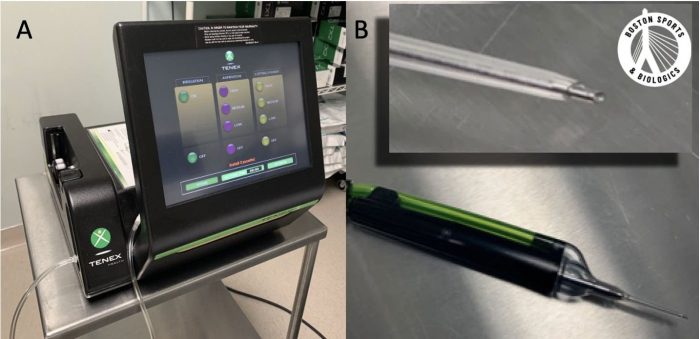
WHAT IS TENEX?
Tenex ultrasound guided needle tenotomy is a treatment for chronic tendon pain. Tenex uses ultrasonic energy to debride and remove abnormal tissue. The Tenex system uses a 19-gage needle, which preferentially removes diseased tendon tissue. The double lumen needle allows the device to irrigate the degenerative tendon with pressurized fluid, and has a vacuum mechanism to remove the fluid and disease tissue.
HOW DOES TENEX WORK?
Resecting the damaged tendon tissue was only previously attainable by performing an open or arthroscopic surgery. Using ultrasound guidance, Tenex precisely targets and removes damaged degenerative tissue. In a basic science study, after removing the pathologic tissue with Tenex new collagen forms and there is normalization of the tendon appearance.[24]
WHAT ARE THE EXPECTED RESULTS?
Tenex provides functional improvement and ultrasound demonstrated tissue repair after Tenex.[25] In a study out of Emory University, PRP and Tenex procedures were both successful in producing clinically and statistically significant improvements in pain, function and quality of life.[26] There was no statistically significant difference between the 2 treatments.
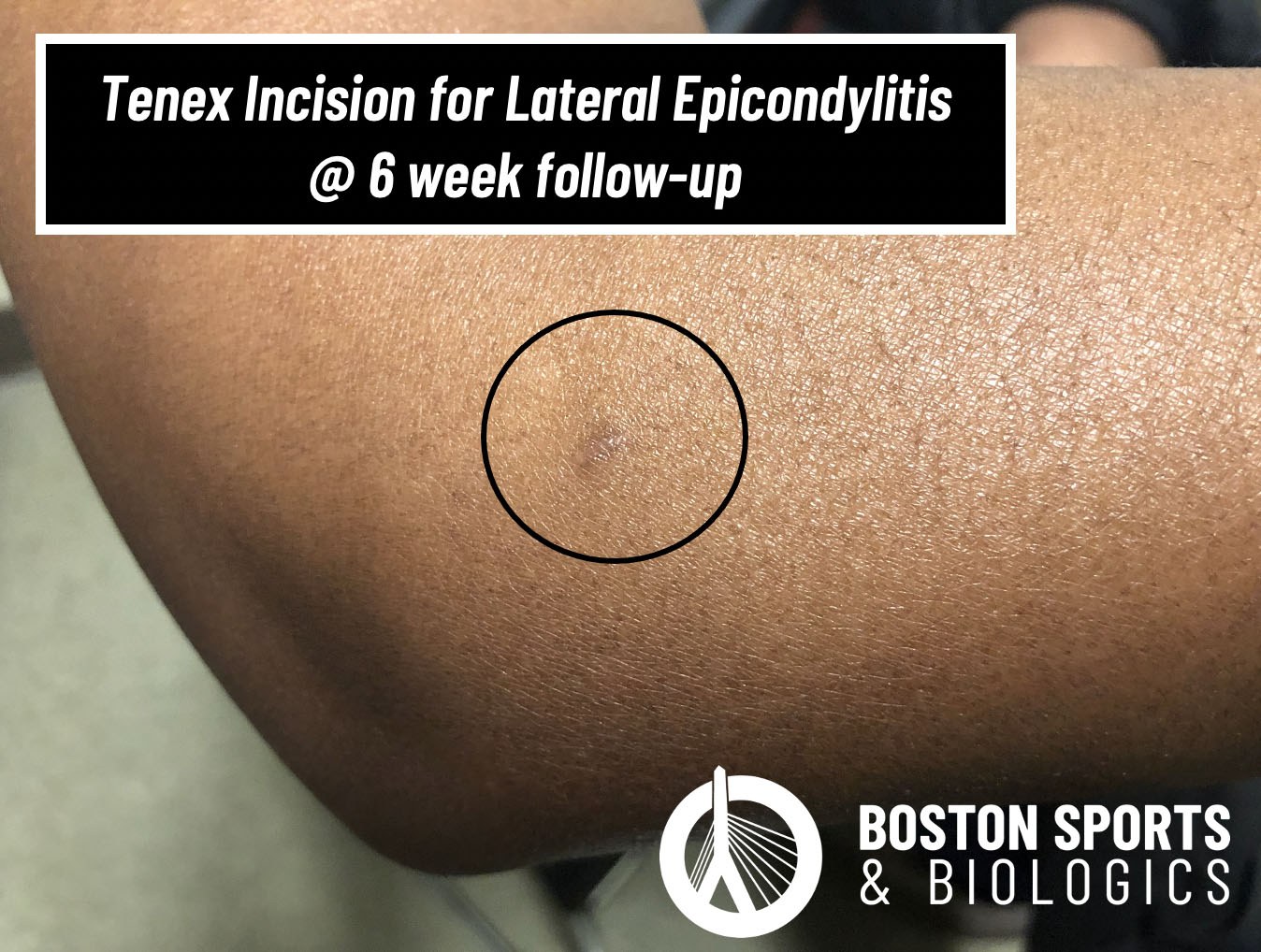
HOW DOES TENEX COMPARE TO SURGERY?
In a study from the Cleveland Clinic and University of Pennsylvania, Tenex and open surgical tenotomy for lateral epicondylitis had similar outcomes at 3-, 6- and 12-months after the procedure.[27] While this study was not powered to assess short term outcomes, Tenex is designed to preserve healthy tendon tissue. Patients can often be cleared to return to work within 2 to 6-weeks after the procedure. In comparison, most surgical protocols place a patient in a cast or splint for 6-weeks after surgery, and only then begin a rehabilitation program.
Restores normal tendon by removing scar tissue
REFERENCES
1. Shiri R, Viikari-Juntura E. Lateral and medial epicondylitis: role of occupational factors. Best Pract Res Clin Rheumatol. 2011; 25(1):43-57.
2. Faro F, Wolf JM. Lateral epicondylitis: review and current concepts. J Hand Surg Am. 2007; 32(8):1271-1279.
3. Coonrad RW, Hooper WR. Tennis elbow: its course, natural history, conservative and surgical management. J Bone Joint Surg Am. 1973; 55(6):1177-1182.
4. Cook JL, Purdam CR. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br J Sports Med. 2009; 43(6):409-416.
5. Sanders TL, Maradit Kremers H, Bryan AJ, Ransom JE, Morrey BF. Health Care Utilization and Direct Medical Costs of Tennis Elbow: A Population-Based Study. Sports health. 2016; 8(4):355-358.
6. Sanders TL, Jr., Maradit Kremers H, Bryan AJ, Ransom JE, Smith J, Morrey BF. The epidemiology and health care burden of tennis elbow: a population-based study. Am J Sports Med. 2015; 43(5):1066-1071.
7. Hodgson RJ, O'Connor PJ, Grainger AJ. Tendon and ligament imaging. The British journal of radiology. 2012; 85(1016):1157-1172.
8. Lee KS. Musculoskeletal sonography of the tendon. J Ultrasound Med. 2012; 31(12):1879-1884.
9. Finnoff JT, Hall MM, Adams E, Berkoff D, Concoff AL, Dexter W, et al. American Medical Society for Sports Medicine (AMSSM) position statement: interventional musculoskeletal ultrasound in sports medicine. PM & R : the journal of injury, function, and rehabilitation. 2015; 7(2):151-168.e112.
10. Byrd JW, Potts EA, Allison RK, Jones KS. Ultrasound-guided hip injections: a comparative study with fluoroscopy-guided injections. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2014; 30(1):42-46.
11. Finnoff JT, Hurdle MF, Smith J. Accuracy of ultrasound-guided versus fluoroscopically guided contrast-controlled piriformis injections: a cadaveric study. J Ultrasound Med. 2008; 27(8):1157-1163.
12. Rozental TD, Zurakowski D, Blazar PE. Trigger finger: prognostic indicators of recurrence following corticosteroid injection. J Bone Joint Surg Am. 2008; 90(8):1665-1672.
13. Benson LS, Ptaszek AJ. Injection versus surgery in the treatment of trigger finger. J Hand Surg Am. 1997; 22(1):138-144.
14. Everding NG, Bishop GB, Belyea CM, Soong MC. Risk factors for complications of open trigger finger release. Hand (N Y). 2015; 10(2):297-300.
15. Finsen V, Hagen S. Surgery for trigger finger. Hand Surg. 2003; 8(2):201-203.
16. Will R, Lubahn J. Complications of open trigger finger release. J Hand Surg Am. 2010; 35(4):594-596.
17. Le ADK, Enweze L, DeBaun MR, Dragoo JL. Current Clinical Recommendations for Use of Platelet-Rich Plasma. Curr Rev Musculoskelet Med. 2018; 11(4):624-634.
18. Deal JB, Smith E, Heard W, O'Brien MJ, Savoie FH, 3rd. Platelet-Rich Plasma for Primary Treatment of Partial Ulnar Collateral Ligament Tears: MRI Correlation With Results. Orthopaedic journal of sports medicine. 2017; 5(11):2325967117738238.
19. Abate M, Verna S, Di Gregorio P, Salini V, Schiavone C. Sonographic findings during and after Platelet Rich Plasma injections in tendons. Muscles, ligaments and tendons journal. 2014; 4(1):29-34.
20. Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med. 2006; 34(11):1774-1778.
21. Karaduman M, Okkaoglu MC, Sesen H, Taskesen A, Ozdemir M, Altay M. Platelet-rich plasma versus open surgical release in chronic tennis elbow: A retrospective comparative study. Journal of orthopaedics. 2016; 13(1):10-14.
22. Bohlen HL, Schwartz ZE, Wu VJ, Thon SG, Finley ZJ, O'Brien MJ, et al. Platelet-Rich Plasma Is an Equal Alternative to Surgery in the Treatment of Type 1 Medial Epicondylitis. Orthopaedic journal of sports medicine. 2020; 8(3):2325967120908952.
23. Ford RD, Schmitt WP, Lineberry K, Luce P. A retrospective comparison of the management of recalcitrant lateral elbow tendinosis: platelet-rich plasma injections versus surgery. Hand (N Y). 2015; 10(2):285-291.
24. Kamineni S, Butterfield T, Sinai A. Percutaneous ultrasonic debridement of tendinopathy-a pilot Achilles rabbit model. Journal of orthopaedic surgery and research. 2015; 10:70.
25. Seng C, Mohan PC, Koh SB, Howe TS, Lim YG, Lee BP, et al. Ultrasonic Percutaneous Tenotomy for Recalcitrant Lateral Elbow Tendinopathy: Sustainability and Sonographic Progression at 3 Years. Am J Sports Med. 2016; 44(2):504-510.
26. Boden AL, Scott MT, Dalwadi PP, Mautner K, Mason RA, Gottschalk MB. Platelet-rich plasma versus Tenex in the treatment of medial and lateral epicondylitis. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al]. 2019; 28(1):112-119.
27. Altahawi F, Li X, Demarest B, Forney MC. Percutaneous ultrasonic tenotomy with the TX-1 device versus surgical tenotomy for the treatment of common extensor tendinosis. Skeletal Radiol. 2020.
Is stem cell therapy better than cortisone for knee arthritis? Learn the differences, risks, benefits, and long-term results of cortisone vs stem cell knee injections.
Read More