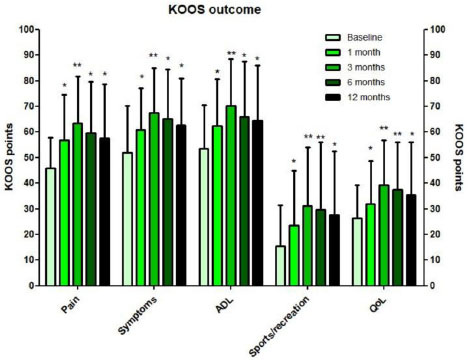
A recent study by Van Genechten et al. evaluated the short-term clinical effect of a single intra-articular autologous MFAT injection for symptomatic knee osteoarthritis. The study enrolled sixty-four subjects with symptomatic mild to severe knee osteoarthritis. Patients received an injection of MFAT into either a single knee (n = 37) or both knees (n = 27).
After liposuction, the adipose tissue was mechanically processed with the Lipogems device. The study defined a positive response to the Lipogems MFAT procedure as a greater than 50% improvement in pain or function. The study demonstrated an early clinical improvement in pain and function, but the response rate was mediocre at 45% at the 12-month follow-up.
When patients with bone marrow lesions on MRI were excluded, the therapeutic responsiveness to the Lipogems MFAT procedure increased to 70% at the 12-months follow-up. Bone marrow lesions, however, did impact the efficacy of the Lipogems procedure. Subchondral bone lesions can cause pain, and since these lesions are located outside the joint, or extra-articularly, it is not a surprise that patients with numerous bone marrow lesions were poor responders to the intra-articular MFAT injection.
Importantly, the severity of the arthritis (i.e. baseline cartilage wear in any compartment) was not found to impact the outcome of the Lipogems MFAT procedure. The authors concluded that “in comparison to repetitive injection therapies such as cortisone, hyaluronic acid, and PRP, administration of MFAT might become a relevant alternative in well-selected patients with symptomatic knee OA.”
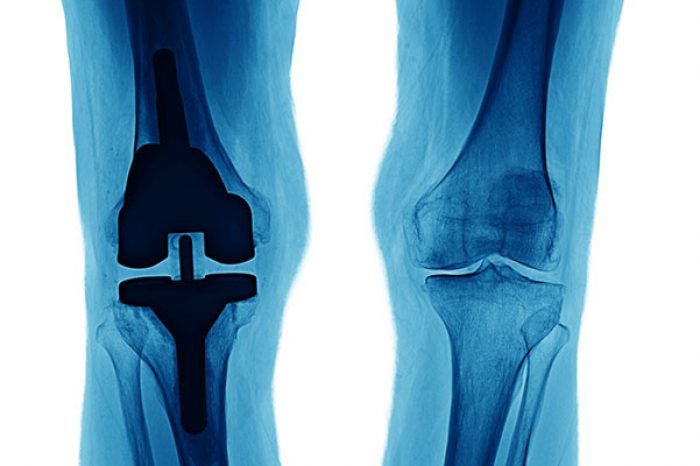
Osteoarthritis is the most prevalent joint disease in the United States with 38–47% of people older than 60 years affected by knee OA (Zhang & Jordan, 2011; Levy et al, 2018). Many patients with symptomatic knee osteoarthritis are considered ‘premature’ for joint replacement surgery, and in these patients minimally invasive conservative therapies are focused on symptomatic relief until these patients are eligible for surgery.
In many patients, intra-articular injection therapies include corticosteroids, hyaluronic acid (HA), platelet-rich plasma (PRP). In patients who remain unresponsive, mesenchymal stromal cells (MSCs) have been considered (Levy et al, 2018), and in this study by Van Genechten et al. the authors concluded that “administration of MFAT might become a relevant alternative in well-selected patients with symptomatic knee OA.”
In Van Genechten et al.'s study, an inflammatory reaction (pain, swelling and stiffness) was reported in the majority of patients with 79% of the subjects in this study reporting at least one of symptom of inflammation in the knees following the Lipogems procedure. The inflammatory reaction resolved spontaneously within 16.6 ± 13.5 days after MFAT administration.
The study demonstrated an early clinical improvement, but a mediocre response rate to a single intra articular injection with autologous MFAT using the Lipogems system. Patients without bone marrow lesions seem to have a better response to MFAT injections.
Studies on the clinical efficacy of MFAT injection in the knee osteoarthritis patient is limited, as and is mainly being provided by small volume case series or case reports, often in combination with arthroscopic lavage procedures (Cattaneo et al, 2018; Panni et al, 2019; Panchal et al, 2018; Borić et al, 2019; Barfod & Blønd, 2019; Franceschini et al, 2016). Fat has a high concentration of reparative cells and is a very powerful tissue. For autologous transplantation purposes, bone marrow and adipose tissue are the two predominant sites for mesenchymal stromal cells (MSCs) harvest, although MSCs from adipose is less invasive and contains a higher relative concentration of MSCs compared to adipose tissue (Tremolada et al, 2016; Damia et al, 2018; Bianchi et al, 2013).
The "clean" Lipogems tissue also provides cushion and support for the area. In accordance with homologous use, the tissue processed in the Lipogems system may be used to facilitate the natural healing process by supporting the repair, replacement or reconstruction of damaged or injured tissue.
Meniscus tears are one of the most common causes of knee pain in active adults and aging athletes alike. If you’ve been told you have a “degenerative meniscus tear,” you may have also heard that surgery isn’t always the
Read MoreFor patients with chronic adductor longus tendinopathy, a newer option is emerging: ultrasound-guided tenotomy using the Tenex system. Recent clinical evidence suggests this minimally invasive approach may effectively
Read More