I recently attended the American Orthopedic Society for Sports medicine (AOSSM) conference in Boston. It brings together some of the thought leaders in the field of sports medicine, and experts from around the world. The conference presented some of the latest research and techniques in the field of sports medicine.
One presentation stood out on the first day of the conference. The University of Pittsburg’s (UPMC) presented the long-term data on the surgical repair of partial hamstring tears with a follow-up average of 6.6 years. They reported low complications rates and all 37 patients being satisfied with the surgery. The biggest down side was the average return to sport was 11-month, over 3 times the recovery seen with platelet rich plasma (PRP) for the same injury.
In comparison, last week we allowed one of our UMass Dartmouh track athletes to return to running at 7-weeks after a PRP injection. I was shocked by the difference in recovery with our athlete versus the expected recover after surgery.
Types of hamstring tears
Three muscles make up the hamstring complex: the biceps femoris (long and short heads), semitendinosus and semimenbranosus. The hamstring originates on the ischial tuberosity. The hamstring crosses both the hip and knee joints, allowing the muscle to flex the knee and extend the hip. Because the hamstring crosses both the hip and knee joints it places it at increased risk.
Hamstring muscle strains are common, and often occur with sport and rapid movements. The hamstring slows knee extension when running or sprinting, and the greatest strain on the hamstring during the swing phase of gait as the muscle elongates. Contracting the muscle at this stage, such as with rapid acceleration and deceleration, can strain the hamstring resulting in tearing of the muscle or tendon.
Hamstring injuries can be subdivided into proximal, muscle belly (myotendinous) and distal injuries. Up to 12% of injuries involve the proximal hamstring tendon. The diagnosis can be confirmed using ultrasound or MRI.
Acute myotendinous junction injury
Injuries most often occur at the myotendinous junction, where the muscle belly and tendon join together. In most cases, myotendinous junction injuries resolve with conservative management.
Complete proximal hamstring avulsion (tendon tear)
If the tear is located within the proximal tendon the recovery can be prolonged. Complete rupture of the tendon sometimes requires surgery, especially when the tendon is pulled away from the bone more than 2cm.
Partial proximal hamstring tear (tendinopathy)
In some cases, the tendon will only partially tear. This can be acute or due to repetitive mild, low-grade micro-trauma. Early on patient often are diagnosed with tendinopathy, but with time this can progress from tendinopathy to a partial tendon tear. Tendon injuries at the enthesis or the junction where the tendon and bone joint have a limited blood supply, potentially impeding the healing process.
Symptoms of Hamstring Injury
Often the symptoms occur acutely, and sometimes patients will feel a popping sensation. Patients will experience pain over the posterior thigh, and sometimes can be associated with bruising.
Patients typically present with lower gluteal pain or posterior thigh pain. Symptoms are typically worse with exercise or sitting, and can limit activity. Reinjury rates are as high as 31% in some studies. In some chronic cases, patients will experience sciatic symptoms if there is scarring of the sciatic nerve.
Treatment options
Treatments for chronic hamstring tendinopathy have been poorly studied, and usually consist of rest, bracing, physical therapy, non-steroidal anti-inflammatory medications, and corticosteroid injections.
Physical therapy
Eccentric strengthening has shown promises in treating tendinopathy, but no randomized controlled trials have specifically looked at eccentric programs for hamstring tendinopathy.
Cortisone (steroid) injections
Historically, steroids have been used in the treatment of tendon pain. Typically steroids will provide a short-term benefit, and for some patients this window of pain relief allows them to rehab the tendon and the pain resolves. Repeated injections may weaken the tendon tissue, and there is concern that tendons could rupture.
Surgery versus Platelet Rich Plasma (PRP)
Surgery
Complete avulsion injuries with retraction of the tendon away greater than >2cm from the bone should be managed surgically. Surgical intervention for complete injuries have shown good to excellent results, but risk include infection, nerve damage, deep vein thrombosis (DVT), wound-related complications and prolonged rehabilitation.
Partial proximal hamstring tears are note as well studied. Only 3 papers reporting outcomes after surgery. The UPMC data showed excellent outcomes, but other studies have not shown similar results.
While UPMC showed 100% patients satisfied, another study showed excellent outcomes in only 69% percent of cases (Lempainen et al, 2006). In another study, only 74% had returned to sport at the 2-year follow up (Aldridge et al, 2012). In that study, 29% of the patients had more pain when sitting than before the surgery.
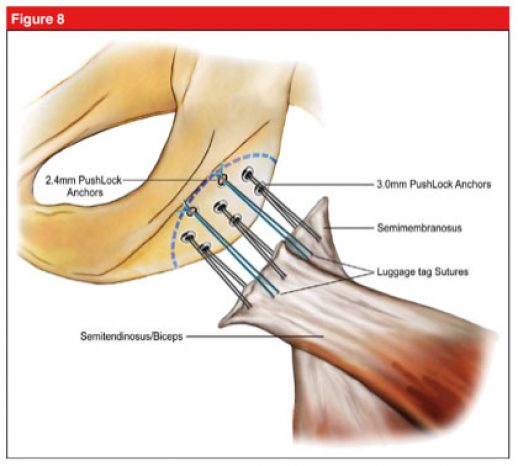
Illustration showing surgical fixation of a proximal hamstring avulsion (Arner et al, 2019)
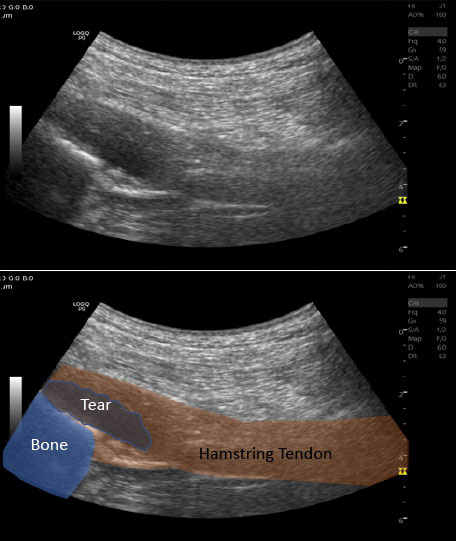
Ultrasound image of partial proximal hamstring tear
Platelet Rich Plasma (PRP)
Platelet rich plasma (PRP) has shown promising results in the literature. PRP is a concentration of a patients own platelets and growth factors (read more). The blood sample is taken in the office, and after it is collected is undergoes centrifugation concentrating the patients own healing factors and is then injected into the partial tear.
PRP has not been shown to increase recovery after an acute hamstring injury, but in chronic cases (patients with >3 months of pain) the literature has shown benefit with PRP. Wetzel et al. first described the use of PRP for hamstring tears in 2013. In 15 patients, patients reported good results with decreased pain at an average of 4.5 months after the PRP injection compared to traditional treatment.
Davenport et al. Showed improved activity of daily living, and decreased pain with sitting after a PRP injection in 17 patients. Fader et al. showed that 80% of patients had decreased pain after a single PRP injection at a 6-month follow up in a series of 18 patients.
In a recent article in Skeletal Radiology, Dr. Park et al. showed PRP to be superior to steroid injections. In 56 patients with grade 2 proximal hamstring injuries, PRP showed decreased pain at 1 and 4-week post-injection. There are major limitations to this study including that they did not collect long-term data and PRP can take a number of months to completely heal the tendon.
PRP versus Surgery – Is there really a choice in partial tears?
PRP is still relatively new in orthopedics with the first reported article for chronic hamstring tears reported in 2013. As the role of PRP in orthopedics continues to expanding, and there is a need for more studies comparing PRP to popular and conventional treatments. Chen has clearly showing PRP to be more effective than steroids. The collegiate athletes we have treated have returned to sports in less than 10 weeks, and I suspect if PRP was compared to surgery in a study, PRP would show decreased recovery time and high patient satisfaction.
For more information schedule a consultation:
References:
Aldridge SE, Heilpern GN, Carmichael JR, Sprowson AP, Wood DG. Incomplete avulsion of the proximal insertion of the hamstring: outcome two years following surgical repair. J Bone Joint Surg Br. 2012;94(5):660-662.
Arner JW1, McClincy MP, Bradley JP. Hamstring Injuries in Athletes: Evidence-based Treatment. J Am Acad Orthop Surg. [Epub ahead of print 2019 Jul 3].
Benazzo F, Marullo M, Zanon G, Indino C, Pelillo F. Surgical management of chronic proximal hamstring tendinopathy in athletes: a 2 to 11 years of follow-up. J Orthop Traumatol 2013; 14:83–89.
Fader RR, Mitchell JJ, Traub S, et al: Platelet-rich plasma treatment improves outcomes for chronic proximal hamstring injuries in an athletic population. Muscles, Ligaments Tendons J 2014;4:461-466.
Karli D, Robinson B. Platelet-rich plasma for hamstring tears. Pract Pain Manag. 2010;10(5):17–18.
Lempainen L, Sarimo J, Heikkila J, Mattila K, Orava S. Surgical treatment of partial tears of the proximal origin of the hamstring muscles. Br J Sports Med. 2006;40(8):688-691.
Lempainen L, Sarimo J, Mattila K, Vaittinen S, Orava S. Proximal hamstring tendinopathy: results of surgical management and histopathologic findings. Am J Sports Med 2009; 37:727–734.
Park PYS, Cai C, Bawa P, Kumaravel M: Platelet-rich plasma vs. steroid injections for hamstring injury-is there really a choice? Skeletal Radiol 2019;48:577-582.
Wetzel RJ, Patel RM, Terry MA. Platelet-rich plasma as an effective treatment for proximal hamstring injuries. Orthopedics. 2013;36(1):e64-70.
Meniscus tears are one of the most common causes of knee pain in active adults and aging athletes alike. If you’ve been told you have a “degenerative meniscus tear,” you may have also heard that surgery isn’t always the
Read MoreFor patients with chronic adductor longus tendinopathy, a newer option is emerging: ultrasound-guided tenotomy using the Tenex system. Recent clinical evidence suggests this minimally invasive approach may effectively
Read More