Gluteal tendinopathy—often called “trochanteric bursitis” or “greater trochanteric pain syndrome”—is a debilitating condition that affects thousands, especially middle-aged women.
Characterized by chronic pain on the outside of the hip, it limits mobility, disrupts sleep, and makes everyday activities a challenge. For those suffering, two major treatment options stand out: Platelet-Rich Plasma (PRP) injections and surgical intervention. But which is more effective?
A recent landmark study by Walker-Santiago (2019) published in the American Journal of Sports Medicine pits PRP against surgery in a head-to-head trial, offering game-changing insights for clinicians, patients, and anyone seeking long-term relief from gluteal tendinopathy.
Before diving into the treatment showdown, it's important to understand the condition itself. Gluteal tendinopathy involves degenerative changes in the gluteus medius and minimus tendons, which attach the gluteal muscles to the hip bone. These tendons play a key role in stabilizing the pelvis and supporting hip movements.
When these tendons are overloaded—due to repetitive motion, poor biomechanics, or aging—they can become inflamed and worn, leading to persistent lateral hip pain. While many people start with conservative treatments like rest, physical therapy, or corticosteroid injections, chronic cases often require more targeted interventions like PRP or surgery [Mellor et al, 2018].
This clinical trial was the first randomized controlled trial comparing PRP injections with surgical intervention for gluteal tendinopathy. It enrolled 99 participants, primarily women over 50, all of whom had failed conservative management for over six months.
Participants were randomly assigned to one of two groups:
PRP Group: Received a single injection of leukocyte-poor PRP.
Surgery Group: Underwent open or endoscopic gluteal tendon repair.
All participants completed a structured post-treatment rehabilitation protocol and were followed for 12 months to assess outcomes.
After a year, both treatment groups reported significant improvements in pain and function. However, the PRP group had slightly better outcomes overall, especially in the early months following treatment. Here’s what stood out:
While surgery can be effective for treating gluteal tendinopathy, it does come with potential risks. According to the study, 10% of patients who underwent surgery experienced complications. These included:
Surgery also involved a significantly longer recovery period—with many patients requiring weeks to months before returning to full activity. In contrast, patients receiving PRP (platelet-rich plasma) injections had no reported complications in this study and were able to recover more quickly.
For patients looking to avoid surgical risks and downtime, PRP may offer a safer, less invasive alternative with fewer side effects and comparable results—especially in the long term.
The results of this study add weight to a growing body of evidence that PRP is a highly effective treatment for chronic tendinopathies. Here’s why it may be preferable to surgery for many patients:
Minimally Invasive: A single injection vs. going under the knife.
Faster Recovery: Less downtime, quicker return to movement and work.
Cost-Effective: Fewer medical costs and no hospital stay.
Lower Risk Profile: Fewer complications compared to surgery.
And perhaps most important, patient satisfaction was higher in the PRP group, particularly in the early recovery phase.
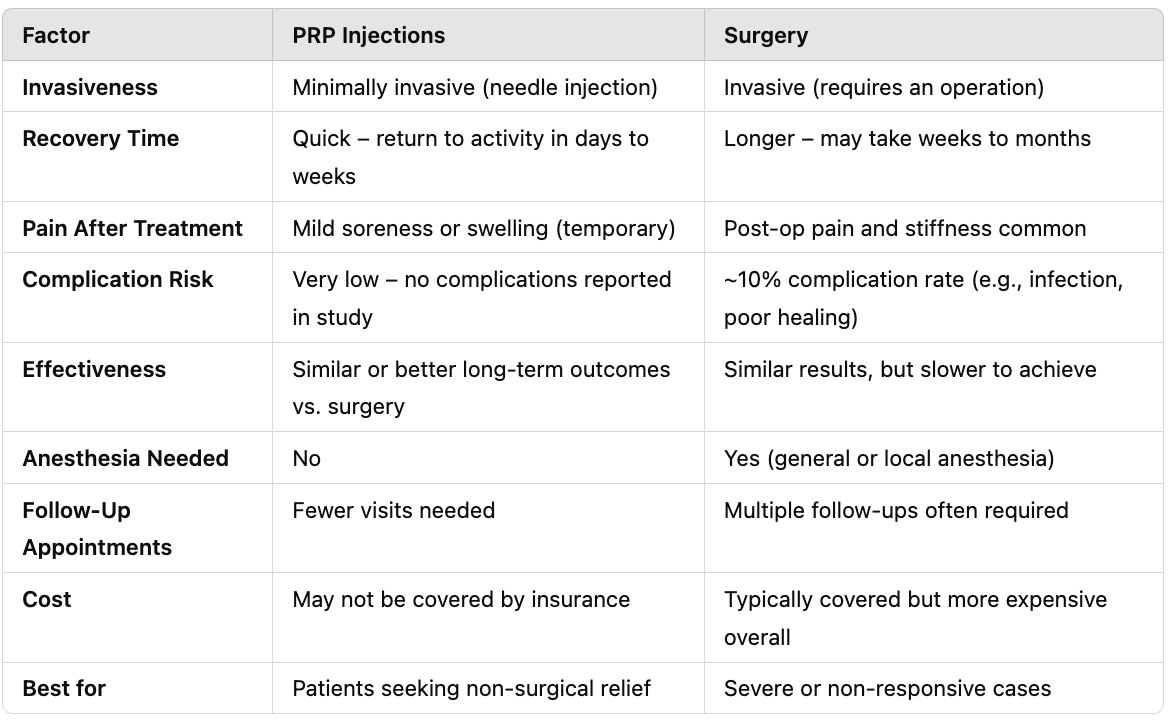
While surgery can still plays a important role for patients who don’t respond to injections or have full-thickness tendon tears, this study highlights that for most chronic gluteal tendinopathy cases PRP can offer equivalent (or superior) outcomes as surgery.
If you're dealing with long-standing lateral hip pain and haven't found relief with physical therapy or steroid injections, PRP may be a good next step—and it might help you avoid surgery altogether.
What you should be asking your provider:
Are you a good candidate for PRP (based on imaging and clinical exam)?
What is the bioformulation (dose) of PRP? (This matters for tendon healing!)
What’s the provider’s experience with PRP for hip conditions?
Do you have a rehabilitation plan post-treatment?
PRP and surgery both significantly reduce pain and improve function in gluteal tendinopathy.
PRP shows better early results, faster recovery, and fewer complications.
PRP may be preferred as a first-line advanced treatment before considering surgery.
Ideal for chronic, non-ruptured tendinopathy cases unresponsive to conservative care.
Looking for relief from hip pain? Want to see if PRP therapy for gluteal tendinopathy is right for you?
(781) 591-7855
20 Walnut St
Suite 14
Wellesley MA 02481
References:
Mellor R, Bennell K, Grimaldi A, Nicolson P, Kasza J, Hodges P, Wajswelner H, Vicenzino B. Education plus exercise versus corticosteroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single blinded, randomised clinical trial. Br J Sports Med. 2018 Nov;52(22):1464-1472.
Walker-Santiago R, Wojnowski NM, Lall AC, Maldonado DR, Rabe SM, Domb BG. Platelet-Rich Plasma Versus Surgery for the Management of Recalcitrant Greater Trochanteric Pain Syndrome: A Systematic Review. Arthroscopy. 2020 Mar;36(3):875-888.
For patients with chronic adductor longus tendinopathy, a newer option is emerging: ultrasound-guided tenotomy using the Tenex system. Recent clinical evidence suggests this minimally invasive approach may effectively
Read MoreAdductor longus selective tenotomy is a modern surgical treatment for chronic groin pain that offers faster recovery and better outcomes than traditional full release surgery. The adductor longus, an inner thigh
Read More