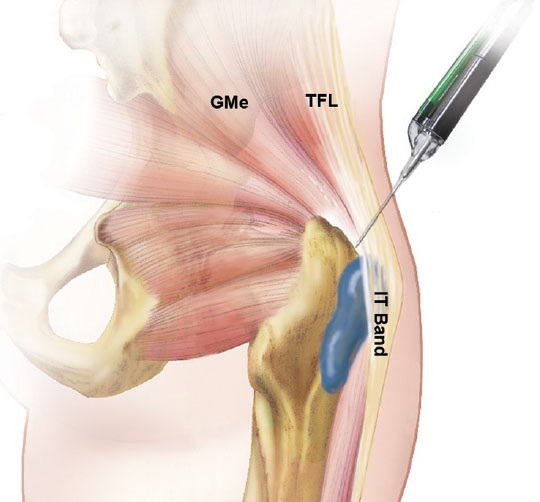
Contrary to the common misconception that symptoms of lateral hip pain are due to underlying "bursitis," the most common cause of lateral hip pain is gluteal tendinopathy due to tendon degeneration and a possible tear of the gluteus medius and/or gluteus minimus tendon (Fearon et al, 2010; Connell et al, 2003; Kingzett-Taylor et al, 1999; Long et al, 2013).
How do you treat hip "bursitis" pain naturally?
Noninvasive treatments for such conditions may include rest, physical therapy with an emphasis on eccentric strengthening, and nonsteroidal anti-inflammatory drugs (Lustenberger et al, 2011).
How do corticosteroid injections work for lateral hip pain or hip bursitis?
Given that the primary cause of pain is tendon degeneration and not inflammation or hip "bursitis" then an intratendinous corticosteroid injections is typically not indicated and predispose the tendon to rupture (Coombes et al, 2010).
Corticosteroid injections have been shown to provide short-term relief of pain associated with gluteus medius tendinopathy, with 72% to 75% of cases reporting positive responses at 4-weeks after the injection (Sayegh et al, 2004; Housner et al, 2009). While cortisone injections have potent anti-inflammatory properties, the high rate of recurrent pain after injecting the "bursa" suggests that cortisone does not address the central underlying cause of lateral hip pain (Rompe et al, 2009; Coombes et al, 2013; Bisset et al, 2006).
The short-term benefit of steroid injections can be attributed to its analgesic effects on local neuropeptides and neurotransmitters that relay pain, (Paavola et al, 2002; Rio et al, 2014) but the long-term destructive (catabolic) consequences associated with corticosteroid injections may outweigh the short-term analgesic benefits (Thomopoulos et al, 2007).
How does dry needling, percutaneous tendon fenestration and Tenex address the cause of hip pain?
Percutaneous tendon fenestration has been used to successfully treat tendinopathy by passing a needle through the area of tendinosis and promoting healing by causing bleeding, which results in an increase in local growth factors and other healing substances (Chiavaras and Jacobson, 2013; Housner et al, 2009; McShane et al, 2006; McShane et al, 2006).
The mechanism of a tenotomy with Tenex is distinct from simply fenestrating the tendon (Baria et al, 2020). Vacuum tenotomy devices such as Tenex effectively cut and simultaneously irrigates the tendon with sterile saline to debrided the tendons without damaging surrounding tissue (Baria et al, 2020). Tenex has been shown to stimulate a healing response with outcomes similar to surgical approaches (Altahawi et al, 2021).
There have been only limited reports that described the use of tendon fenestration and tenotomy around the hip and pelvis, but the available studies show positive outcomes (Baker and Mahoney, 2020; Jacobson et al, 2015; Jacobson et al, 2016).
What is the evidence for Tenex for chronic gluteal tendon pain?
In a case series, 29 patients with chronic lateral hip from chronic gluteal tendinopathy underwent a tenotomy using the Tenex device. The patients were followed for 22-months after the procedure. The
majority of patients had a clinically significant decreased in pain and
improved function and 90% of patients were able to avoid an
open surgery.
Only 10% of patients failed the tenotomy procedure and required surgery for
continued pain.
Meniscus tears are one of the most common causes of knee pain in active adults and aging athletes alike. If you’ve been told you have a “degenerative meniscus tear,” you may have also heard that surgery isn’t always the
Read MoreFor patients with chronic adductor longus tendinopathy, a newer option is emerging: ultrasound-guided tenotomy using the Tenex system. Recent clinical evidence suggests this minimally invasive approach may effectively
Read More