Calcific tendinitis is when “calcium deposits” form within the tendon. These calcifications can form anywhere within the body. Calcifications do not always cause pain, but 7% of cases of shoulder pain are caused by calcifications in the tendon (Speed & Hazleman, 1999).
What causes calcifications in the shoulder?
No one knows why calcifications form, but different theories have been proposed.
Some think that the calcifications are a response to microtrauma to the tendon. Others have suggested the calcium deposits form when there is not enough oxygen to the tendon.
What are the symptoms of calcific rotator cuff tendinopathy?
When the calcifications are forming patients may not feel any pain, and studies show that calcifications are seen in 7.8% of healthy, or asymptomatic shoulder (Louwerens et al, 2015). This means that when physicians perform x-rays of someone’s shoulders we sometimes see calcifications … even when that person does not have any pain. When the body starts to reabsorb the calcification the shoulder can become incredibly painful. Patients will often report pain that interferes with sleep, and worsens with shoulder movement.
How is rotator cuff calcifications diagnosed?
Calcifications are often diagnosed by x-ray. X-rays protocols vary and calcifications can be easily missed. Even with magnetic resonance imaging (MRI), calcifications can be falsely interpreted as a rotator cuff tear.
Ultrasound has been shown to be very sensitive in detecting calcium deposits within the rotator cuff, with a sensitivity of 100% and specificity of up to 98% (Ottenheijm et al, 2010).
What is a shoulder barbotage procedure?
Barbotage, or lavage, is a way to wash out or irrigate the calcification and remove it. The procedure uses ultrasound to guide a needle into the deposit and the calcification loosened and removed through the needle. It is hard to argue that ultrasound guided aspiration of calcifications is a novel technique. Farin et al first described the approach in 1996, and it has been shown to be effective, quick and less expensive than arthroscopic surgery. In some studies, 91% of shoulders had complete resolution of symptoms (del Cura et al, 2007).
X-ray showing a large rotator cuff calcification.

Will shoulder calcifications go away?
Often calcifications will resorb over time, but the length of symptoms can be unpredictable. In one study, at 3 years dense deposits disappeared in 33% of cases and fluffy deposits resorbed in 71% of cases (Gartner & Simons, 1990).
The problem is that the resorptive phase can be incredibly painful, and the time required for the calcifications to spontaneously disappear is so long that it can adversely affect a patients quality of life.
What is the treatment for calcific tendonitis?
Most of the time calcific tendonitis can be treated non-operatively with ice, rest and pain medications. Mild cases can respond to physical therapy or steroid injections. Lithotripsy and extra-corpeal shock wave therapy have also been used, but often can require multiple treatments and can be painful.
In 27% of cases (Ogon et al, 2009) patients will continue to have pain despite conservative management. In these cases, you can remove the calcification with ultrasound guided barbotage, or lavage.
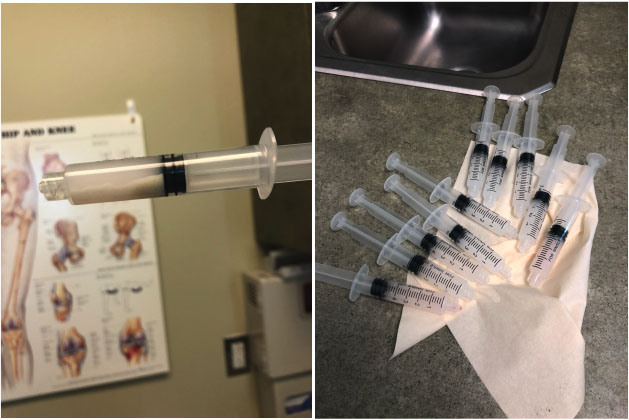
Microcalcifications aspirated with a barbotage procedure.
Do I really need surgery to remove the calcification in my Rotator Cuff?
If
the calcification can be visualized on ultrasound we can treat it
we a percutaneous approach and often can help patients avoid an open
surgery. Arthroscopic surgery to debride rotator cuff calcification is a
dependable procedure, and ultrasound guided aspiration of
calcifications is the standard of care.
Surgery requires general anesthesia and has been associated with complications such as tendon ruptures. If you have only been offered surgery for your calcification it is likely that your orthopedic surgeon does not perform the minimally invasive procedure and/or is not up to date with the literature.

Close up photo of the Tenex needle.
Advances in calcific tendinopathy treatment?
We are now performing the barbotage procedure with Tenex. It allows
us to perform the procedure in under 5 minutes with local numbing around
the tendon and calcification. The means you are awake during the
procedure, and do not need general anesthesia.
The Tenex needle use ultrasonic energy to break apart the calcification, and the calcium debris is sucked through the inner lumen and out of the shoulder.
Patients are not immobilized after the procedure and are allowed
to return to normal activity following the procedure with only a
Band-Aid over the procedure site. Why would you undergo the risk of
general anesthesia when a simple minimally invasive procedure has
similar outcomes?
Complete resolution of pain can sometimes take a few months, and most shoulder calcifications resolve within 3-4 months of the procedure.
Tenex for Calcific Rotator Cuff Tendinopathy
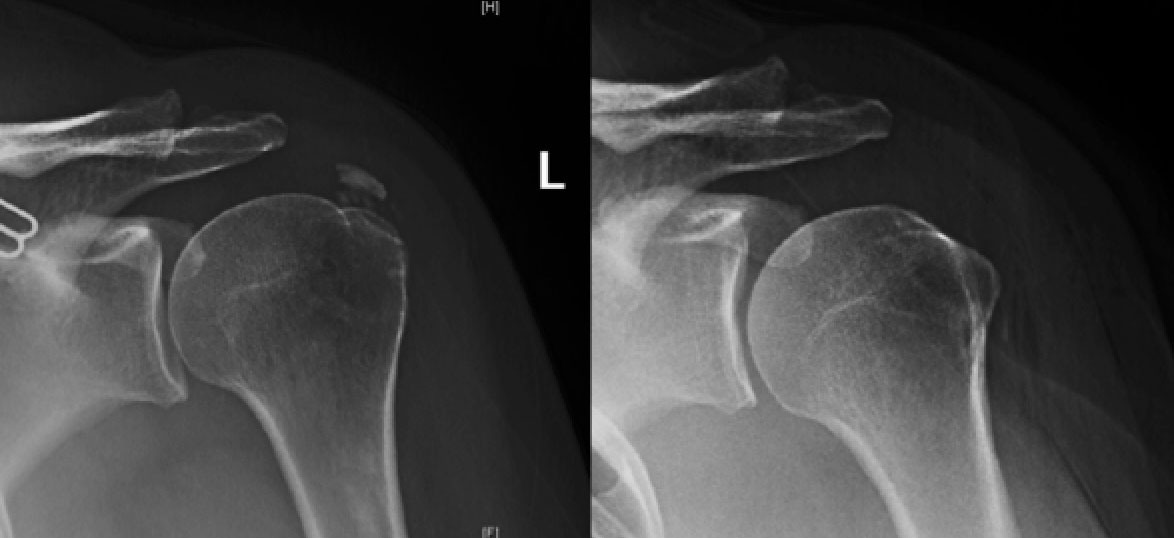
These are x-ray of one of our patients who had a minimally invasive procedure to remove a calcification in her rotator cuff. The x-ray on the left was taken immediately after the procedure showing resolution of the calcification.
How can I determine if I am a candidate for a barbotage procedure?
If you have been diagnosed with calcifications in the shoulder or rotator cuff you may be a candidate for a shoulder barbotage procedure. X-rays and an examination will often confirm the diagnosis.
Minimally invasive procedures are often performed by an interventional radiologist or sports medicine physician trained in ultrasound guided procedures. Call (781) 591-7855 to schedule a consultation.
Can calcifications occur outside the shoulder?
The majority of calcifications within tendons occurs in the shoulder, but calcific tendinitis can occur within any tendon in the body. Calcification within tendons can be mis-diagnosed as tennis elbow, hip bursitis and Achilles tendonitis. If the calcification can be visualized on ultrasound we can treat it we a percutaneous approach.
Shoulder barbotage is less invasive than surgery so you will recover more quickly, you will not need general anesthesia or "sleeping medicine" and has a high success and low complication rate.
References:
del Cura JL, Torre I, Zabala R, Legorburu A. Sonographically Guided Percutaneous Needle Lavage inCalcific Tendinitis of the Shoulder: Short- and Long-Term Results. AJR 2007; 189:W128–W134.
Farin PU, Jaroma H, Soimakallio S. Rotator cuff calcifications: treatment with US-guided technique. Radiology 1995; 195(3): 841–843.
Gartner J, Simons B. Analysis of calcific deposits in calcifying
tendinitis. Clin Orthop Relat Res 1990;(254):111-20.
Louwerens JK, Sierevelt IN, van Hove RP, et al. Prevalence of calcific deposits within the rotator cuff tendons in adults with and without subacromial pain syndrome: clinical and radiologic analysis of 1219 patients. J Shoulder Elbow Surg. 2015 Oct;24(10):1588-93.
Speed CA, Hazleman BL. Calcific tendinitis of the shoulder. N Engl J Med 1999; 340:1582–1584
Ogon P, Suedkamp NP, Jager M, et al. Prognostic Factors in Nonoperative Therapy for Chronic Symptomatic Calcific Tendinitis of the Shoulder. Arthritis Rheum 2009;60:2978-84.
Ottenheijm RP1, Jansen MJ, Staal JB, et al. Accuracy of diagnostic ultrasound in patients with suspected subacromial disorders: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2010 Oct;91(10):1616-25.
Is stem cell therapy better than cortisone for knee arthritis? Learn the differences, risks, benefits, and long-term results of cortisone vs stem cell knee injections.
Read More