Alternatives to Surgery for Chronic Tennis Elbow
According to a study in the American Journal of Sports Medicine, about 1 in 10 patients with persistent tennis elbow end up having surgery. The number of cases treated surgically has actually gone up, tripling between 2000 and 2009.
So why has the number of cases in our practice actually decreased? Despite having 2 hand surgeons in our practice, surgery for tennis elbow is uncommon. In today’s world with advances in regenerative medicine and minimally invasive procedures patients now have a lot of options to help them avoid surgery. These new procedures have similar outcomes as traditional surgical procedures without the risk of anesthesia or the long recovery.
What is Tennis Elbow?
Tennis elbow, or lateral epicondylitis, is one potential cause of pain over the outside or lateral elbow. The tendon that attaches to the outside of the elbow extends the fingers and wrist.
Once thought to be a result of inflammation, research has shown that tennis elbow is due to degeneration or partial tearing of the common extensor tendon. These injuries to the tendon are often from overuse and gradual ward and tear. Often there is no specific injury, but symptoms can worsen with activity.
Patients will typically report pain or burning over the outside of the elbow. Weak grip strength is common.
What are my treatment options?
Conservative Treatment
In the majority of cases tennis elbow resolves over time with conservative management, including physical therapy, non-steroidal anti-inflammatory medications (i.e. Motrin, ibuprogen, Aleve, naproxen), and cortisone (steroid) injections.
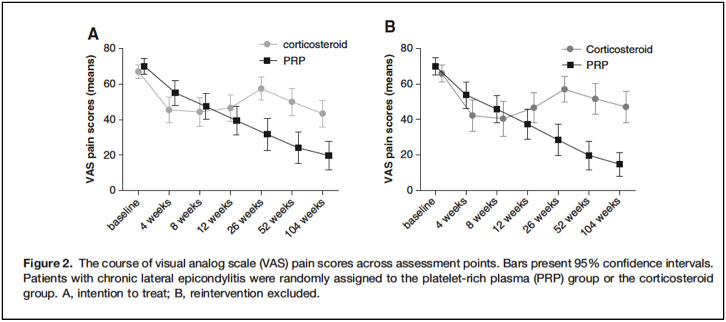
Recent studies have shown that cortisone injections can help for a few months, but may inhibit healing long-term. Studies have shown that cortisone injections can kill healthy tendon cells, and may actually make tennis elbow worse in the long run. In a study by Coombes et al. in the Journal of the American Medical Association (JAMA), patients that receive a cortisone injection do worse at the one-year follow-up than those that receive a placebo injection.
Tenex
Percutaneous needle tenotomy was first described by McShane et al in 2006, and involved repeatedly fenestrating the diseased tendon. This disrupted the abnormal tendon and stimulated a healing response.
The Tenex needle uses ultrasonic technology to peform the tenotomy, and has a high rate of success when compared to a simple percutaneous needle tenotomy. The first study looking at Tenex by Koh et al. in 2013 showed that 95% of patients were satisfied with the procedure.
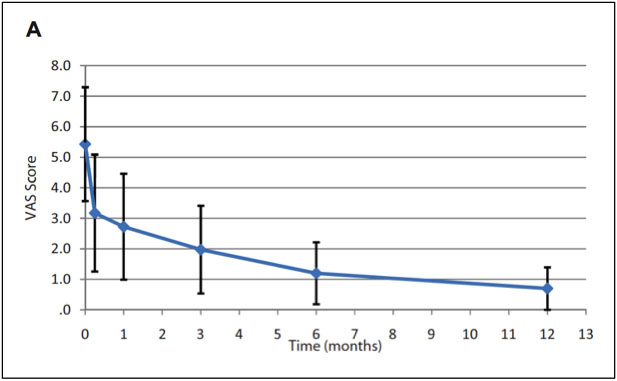
We have performed more Tenex procedures than any clinic or physician in all of New England. Tenex is typically covered by insurance. The Tenex procedure is done with only local anesthesia and patients are allowed to return to normal activity immediately following the procedure. Tenex can precisely target abnormal portions of the tendon without cutting healthy tendon tissue. Tenex has similar outcomes to traditional open surgery (Altahawi et al 2020), but after surgery patients are often immobilized in a cast or splint for 6-weeks.
Platelet Rich Plasma (PRP)
One of the best-studied treatments for tennis elbow is platelet rich plasma (PRP) injections. PRP is performed in the office, involves taking blood from a vein in the arm, concentrating the platelets in a centrifuge and injecting the PRP in to the tears within the tendon. Unlike cortisone injections, PRP should not wear off and will hopefully heal the tendon. When comparing PRP to steroids, Gosens et al. showed PRP to be more effective.
There are 36 commercial kits available to clinicians to make PRP. There are large differences in the quality of the PRP these kits produce. In addition to making sure you get the highest quality of PRP, you want to make sure the PRP is injected into the tears within the tendon. Using ultrasound to guide the PRP into the tears is critical to the success of the treatment.
Rehabilitation
Gradual strengthening exercises are important to conditioning the tendon after Tenex or PRP. In many cases, patients are not adequately instructed on what to do after a regenerative or biologic procedure. We have published a large review on the rehabilitation protocol after these procedures (Sussman et al, Regen Medicine), and will instruct you on the right exercises to maximize the chance of success.
Reference
Altahawi F, Li X, Demarest B, Forney MC. Percutaneous ultrasonic tenotomy with the TX-1 device versus surgical tenotomy for the treatment of common extensor tendinosis. Skeletal Radiol. 2020.
Coombes BK, Bisset L, Brooks P, et al. Effect of corticosteroid injection, physiotherapy, or both on clinical outcomes in patients with unilateral lateral epicondylalgia: a randomized controlled trial. JAMA. 2013 Feb 6;309(5):461-9.
Gosens T1, Peerbooms JC, van Laar W, et al. Ongoing positive effect of platelet-rich plasma versus corticosteroid injection in lateral epicondylitis: a double-blind randomized controlled trial with 2-year follow-up. Am J Sports Med. 2011 Jun;39(6):1200-8.
Koh JS, Mohan PC, Howe TS, et al. Fasciotomy and surgical tenotomy for recalcitrant lateral elbow tendinopathy: early clinical experience with a novel device for minimally invasive percutaneous microresection. Am J Sports Med. 2013 Mar;41(3):636-44.
Sanders TL, Kremers HM, Bryan AJ, eta al. The Epidemiology and Health Care Burden of Tennis Elbow:A Population-Based Study. Am J Sports Med. 2015 May; 43(5): 1066–1071.
Sussman WI, Mautner K, Malanga G. The role of rehabilitation after regenerative and orthobiologic procedures for the treatment of tendinopathy: a systematic review. Regen Med. 2018 Mar;13(2):249
Historically, osteoarthritis was described as “wear and tear” of cartilage. We now understand it as a whole-joint disease, involving cartilage breakdown, subchondral bone remodeling, and bone marrow lesions. In recent
Read More