
Trigger finger surgery is common but patients miss on average 2-3 weeks of work. Ultrasound guided percutaneous trigger finger release can result in fewer days of work missed and better cosmetic results than open surgery.
I just finished editing a chapter on the percutaneous release of trigger fingers for our upcoming book on Interventional Orthopedics to be published in 2020 by Elsevier. The chapter was written by Dr. Ricardo Colberg of the Andrews clinic in Alabama, and reviews how to perform the minimally invasive procedure.
While surgery for trigger finger is reliable and minimally invasive, the percutaneous approach requires not stitches, offers a faster recovery and patient’s return to work in days instead of weeks.
What is a trigger finger?
The finger flexors tendons that bring the fingers toward the palm are held into place by a pulley system. The pulleys, or annular pulleys, keep the tendons in place and prevent them from bunching up. The pulleys are numbered proximal to distal from A1 to A5.
Trigger finger occurs when the tendon or pulley becomes thickened, narrowing the tunnel the tendon runs through. This can cause catching of the tendon as it glides through the pulley. In mild cases, patients can experience pain and catching. In severe cases, the tendon can lock and get stuck.
Why do people get trigger finger?
In most cases, we don’t know why people get a trigger finger. Repetitive microtrauma is thought to be the main risk factor. Trauma, diabetes, rheumatoid arthritis and hypothyroidism can predispose or increase the risk of developing a trigger finger.
How is trigger finger diagnosed?
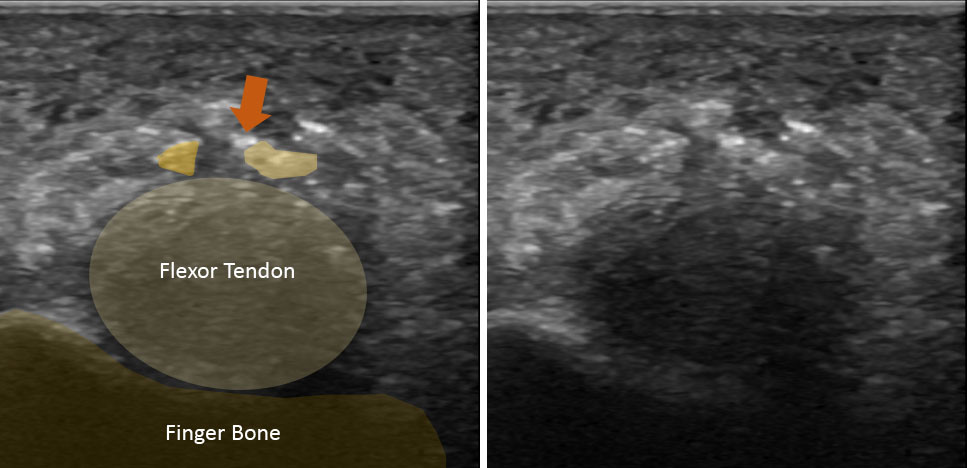
Often trigger finger is a clinical diagnosis, but the diagnosis can be confirmed with ultrasound. Ultrasound can accurately assess any changes to the pulley or tendon, and rule out any secondary causes for the triggering (ie a cyst or bone spur).
How are trigger fingers treated?
In the majority of cases, trigger fingers resolve without any treatment. In a study by McKee et al, 52% of cases resolved at 8 months from the initial visit. Treatment usually starts with anti-inflammatory medications (NSAIDs), finger night splints, cortisone injection, and/or physical therapy.
Surgery is often recommended for cases that do not respond to conservative management (Ma et al, 2018). Trigger finger release is the 2nd most common hand surgery behind only carpal tunnel release (Veltre et al, 2019). However, in a recent Cochrane review the benefits of surgery were uncertain (Fiorini et al 2018). Other articles also showed no significant difference in pain relief between patients treated with steroid injections and those treated with surgery at 3 months after the treatment (Hansen et al, 2017; Zyluk et al).
Do I have alternatives to an open surgery?
Surgery is often a last resort for patients, and percutaneous trigger finger release is an alternative to open surgery. Percutaneous trigger finger release is a quick procedure, less painful, and has shown significantly better results in rehabilitation than open surgery (Gilberts et al, 2001; Dierks et al 2008).
Nikolaou et al. compared ultrasound guided trigger finger release to open surgery. In the ultrasound guided release, 93.75% (15/16) of cases were successful compared to 100% (16/16) of open surgical cases. The ultrasound guided percutaneous release group, however, returned to normal activities at an average of 4.1 days compared to 17.8 days after an open surgery. The cosmetic results of the percutaneous release group were also superior.
Nikolaou et al. (2017) compared ultrasound guided trigger finger release to open surgery. In addition to the ultrasound percutaneous release group returning to work in an average of 4.1 days, the patients were happier with the cosmetic results.
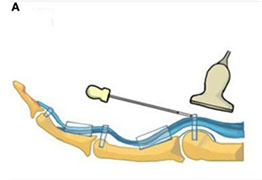
How is an ultrasound guided percutaneous trigger finger release performed?
An ultrasound guided percutaneous trigger finger release is different than a traditional percutaneous release. Ultrasound guidance allows the physician to visualize the thickened tendon and A1 pulley. The physician can direct a specially designed needle to the A1 pulley, cutting the pathologic tissue.
If done correctly, patients should not feel any residual catching/locking after the procedure and rate of recurrence is less than 1% (Salim et al 2012). The cosmetic results are better with the percutaneous procedure and return to work is faster (Nikolaou et al 2017).

What are the risks of a percutanous release compared to open surgery?
The risks of a percutaneous release are similar to complications of open surgery or cortisone injections (Bruijnzeel et al, 2012). Laceration of the tendon has been reported in 13% of cases treated with percutaneous release (Gulabi et al, 2014). Ultrasound minimizes the risk associated with a percutaneous release.
Reference:
Bianchi S, Gitto S, Draghi F. Ultrasound Features of Trigger Finger: Review of the Literature. J Ultrasound Med. 2019 May 20. [Epub ahead of print]
Fiorini HJ, Tamaoki MJ, Lenza M, et al. Surgery for trigger finger. Cochrane Database Syst Rev. 2018 Feb 20;2:CD009860.
Hansen RL, Søndergaard M, Lange J. Open Surgery Versus Ultrasound-Guided Corticosteroid Injection for Trigger Finger: A Randomized Controlled Trial With 1-Year Follow-up. J Hand Surg Am. 2017 May;42(5):359-366.
Ma S, Wang C, Li J, et al. Efficacy of Corticosteroid Injection for Treatment of Trigger Finger: A Meta-Analysis of Randomized Controlled Trials. J Invest Surg. 2018 Jan 30:1-9. [Epub ahead of print]
McKee D, Lalonde J, Lalonde D. How Many Trigger Fingers Resolve Spontaneously Without Any Treatment? Plast Surg (Oakv). 2018 Feb;26(1):52-54.
Nikolaou VS, Malahias MA, Kaseta MK, et al. Comparative clinical study of ultrasound-guided A1 pulley release vs open surgical intervention in the treatment of trigger finger. World J Orthop. 2017 Feb 18;8(2):163-169.
Pan M, Sheng S, Fan Z, et al. Ultrasound-Guided Percutaneous Release of A1 Pulley by Using a Needle Knife: A Prospective Study of 41 Cases. Front Pharmacol. 2019 Mar 26;10:267. eCollection 2019.
Veltre DR1, Yakavonis M1, Curry EJ1, et al. Regional Variations of Medicare Physician Payments for Hand Surgery Procedures in the United States. Hand (N Y). 2019 Mar;14(2):209-216.
Zyluk A, Jagielski G. Percutaneous a1 pulley release vs steroid injection for trigger digit: the results of a prospective, randomized trial. J Hand Surg Eur Vol. 2011;36:53–56.
Platelet-rich plasma (PRP) has become one of the most discussed treatments in sports medicine and orthobiologics. It’s used for knee osteoarthritis, tendinopathy, muscle injury, and more. But despite its growing
Read MoreMeniscus tears are one of the most common causes of knee pain in active adults and aging athletes alike. If you’ve been told you have a “degenerative meniscus tear,” you may have also heard that surgery isn’t always the
Read More