In a 2017 study, Dr. Mike Baria et al. and a team of nonoperative sports medicine physicians at the Mayo Clinic studied the feasibility of percutaneous intrameniscal injections to deliver these biologic agents into the meniscus (Baria et al, 2017). A total of 20 intrameniscal injections were performed in 5 cadaveric specimens. Colored latex dye was used to confirm the accuracy of these injection. In 17 injections the dye was placed in the desired location in the meniscus. In 2 cases, dye was seen in the posterior horn of the meniscus instead of the target location in the body of the meniscus. These inaccuracies resolved with modification to the authors technique. None of the specimens had evidence of injury to the adjacent nerves, arteries or cartilage.
This study demonstrated that intrameniscal injections are feasible and that injections of biologics can be safely placed across the full width of the meniscus, including the innermost portion of the bodies and posterior horns of the medial or lateral meniscus.
In this study, 85% of the injections accurately were placed in the desired location (Baria et al, 2017).. In 2 cases the injection was placed in the posterior horn instead of the body of the meniscus. In 1 case the dye was thought to have clogged the needle and was not seen in the meniscus. Overall, ultrasound guided injections into the meniscus are accurate.
This is important clinically, as this technique provides an accurate way to inject orthobiologics into the meniscus.
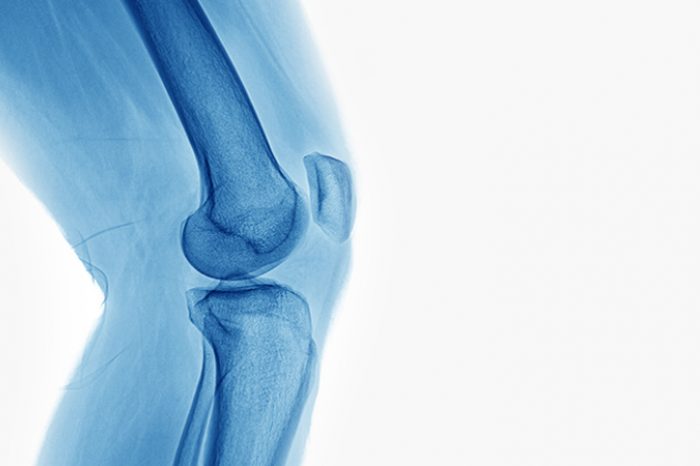
Not all meniscus tears cause pain and dysfunction, but in cases where a meniscus tear is causing you pain we can precisely target the damaged or torn area of the meniscus using ultrasound. Orthobiologic injections, including platelet rich plasma (PRP) injections, bone marrow aspirate concentrates and mesenchymal stem cells or stromal cells (MSCs) have been proposed to improve pain and promote meniscal regeneration.
The most common surgery for a degenerative meniscal tear is a partial meniscectomy, which involves removing part of the meniscus. Limitations include that in studies this surgery has been found to be no better than physical therapy (Beaufils et al, 2017) or a sham surgery (Sihvonen et al, 2013) in degenerative meniscus. Surgery also places the patient at risk for early onset arthritis and a higher chance of needing a knee replacement (Katz et al 2019).
Meniscal tears are common and the trend is to offer treatments that preserve the meniscus. Learn more about alternatives to surgery.
Bone marrow aspirate concentrate, or BMAC, is a safe and reliable source of mesenchymal stem cells (MSCs), and one of the few forms of stem cell delivery in compliance with the US FDA guidelines.
Lipogems or micro-fragmented adipose tissue (MFAT) is one method of harvesting mesenchymal stromal cells or stem cells (MSCs). Learn more about how Lipogems is performed here.
To learn more about nonoperative procedures for meniscus tears call for consultation to see if you are a candidate. Contact us at:
Meniscus tears are one of the most common causes of knee pain in active adults and aging athletes alike. If you’ve been told you have a “degenerative meniscus tear,” you may have also heard that surgery isn’t always the
Read MoreFor patients with chronic adductor longus tendinopathy, a newer option is emerging: ultrasound-guided tenotomy using the Tenex system. Recent clinical evidence suggests this minimally invasive approach may effectively
Read More