A meniscus tear is an injury to the meniscus, which is a C-shaped cartilage cushion in the knee that acts as a shock absorber between the two bones in the knee joint (the femur and tibia). There is a medial (inside of the knee) and a lateral (outside of the knee) meniscus.
The degree of meniscus injury can vary. Meniscus tears can occur due to an acute injury or trauma, often involving a twisting motion of the knee, or due to degenerative changes in older adults [Abram et al, 2018].
Typical Symptoms include:
Knee pain, particularly along the joint line.
Swelling and stiffness.
Mechanical symptoms such as locking, catching, or giving way of the knee.
Difficulty bending and straightening the knee fully.
Clinical Evaluation Methods:
A detailed history and physical examination are crucial. Key clinical tests also suggest a meniscal tear.
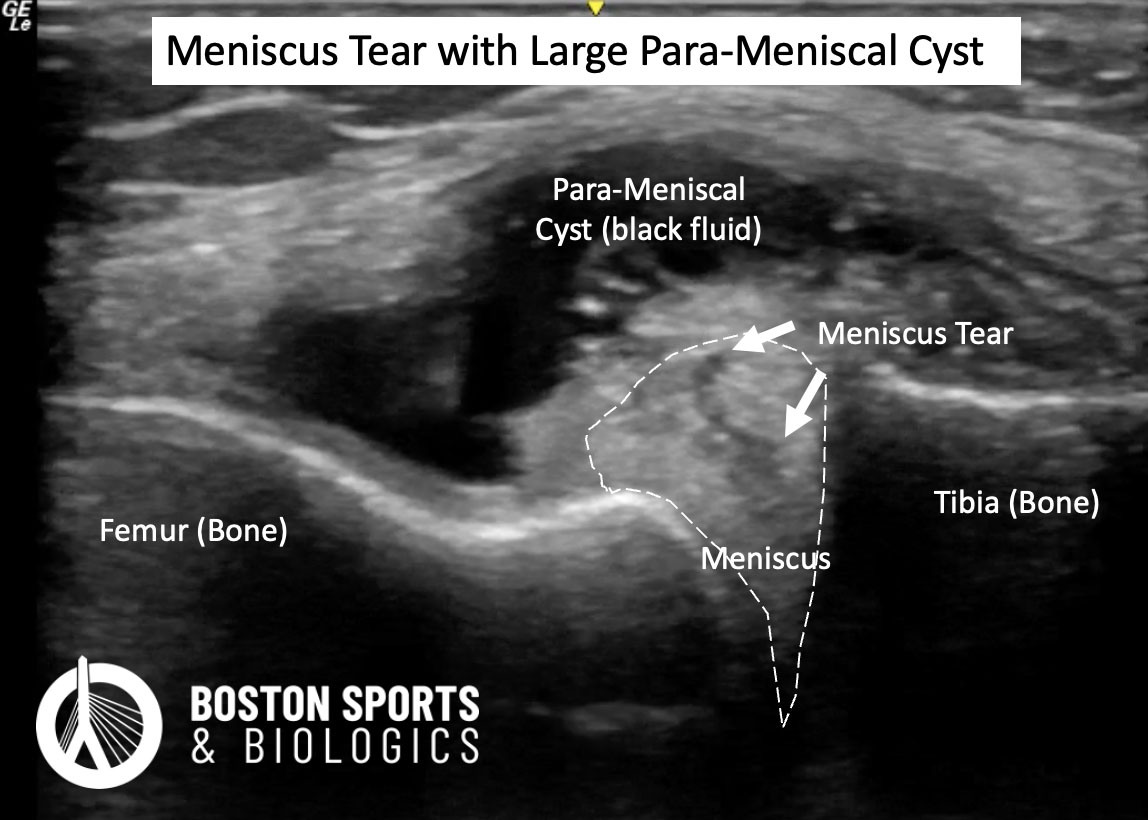
The diagnosis can be confirmed with MRI or ultrasound.
Conservative treatment
Conservative
treatment options for meniscal tears, including rest, physical therapy,
and nonsteroidal anti-inflammatory drugs (NSAIDs), have been shown to
be effective and are often comparable to surgical interventions in many
cases.
A
meta-analysis by Lee et al. found no significant differences in
clinical outcomes such as knee pain relief and improved knee function
between arthroscopic meniscal surgery and conservative management in
patients aged 40 years and older [Lee et al, 2018]. Additionally, the five-year follow-up of the ESCAPE trial confirmed
that exercise-based physical therapy remained noninferior to APM for
patient-reported knee function, suggesting that PT should be the
preferred treatment over surgery for degenerative meniscal tears [Noorduyn et al, 2022].
Non-surgical treatment includes activity modification (i.e. avoiding deep squats and twisting/pivoting activities), medications, physical therapy, braces and steroid or viscosupplemention injections.
Orthobiologic Treatment
Surgical Treatment
Evidence supporting surgical intervention for meniscal tears is mixed and context-dependent. When considering surgical options understanding the type of tear and symptoms is important in predicting outcomes. Traumatic meniscal tears are often viewed as a different injury than degenerative meniscal tears, and surgery is often offered for traumatic meniscal tears with the hope of providing short-term benefit.
Short-term Benefits: Arthroscopic partial meniscectomy (APM) has been shown to provide small, statistically significant improvements in physical function and pain relief at 2 to 6 months after the surgery when compared to conservative treatments, but these differences were not sustained at 12 and 24 months [van de Graaf, 2016].
Learn more about minimally invasive treatment
options for chronic degenerative meniscus tears here.
(781) 591-7855
20 Walnut St
Suite 14
Wellesley MA 02481
Autologous platelet rich plasma (PRP) injections release multiple growth factors, cytokines and other signaling proteins that play an important role in healing. PRP has been shown to help partially or full heal the meniscus on MRI in 60% of patients.
Adult mesenchymal stem cells derived from bone marrow aspirates showed evidence of meniscus regeneration and improved pain
Lipogems or micro-fragmented adipose tissue (MFAT) injections include mesenchymal stem cells (MSCs) harvested from adipose tissue and act as trophic mediators to stimulate differentiation of tissue intrinsic stem cells or reparative cells. MFAT has shown encouraging results as a lipofiller in degenerative meniscal tears.
References
(781) 591-7855
20 Walnut St
Suite 14
Wellesley MA 02481