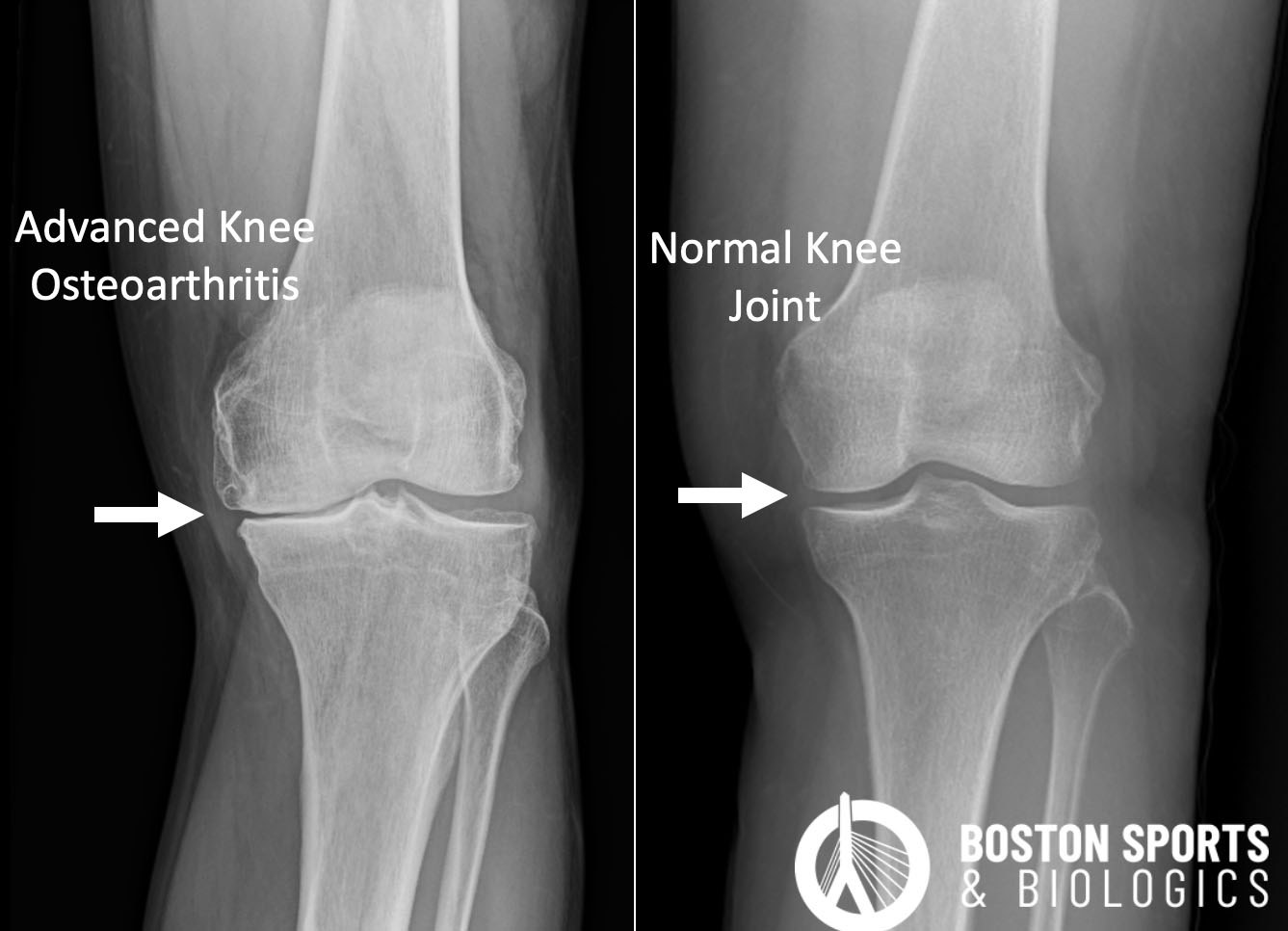
What are the treatments for Knee Arthritis?
Nonsurgical options historically included:
Many patients are not ready for a joint replacement and there are a number of strategies to help manage pain until you are ready or the disease is severe enough to warrant surgery. The goal of treatment is to control the pain. Various evidence supports medications, weight loss, bracing, physical therapy, and cortisone injections.
- Pharmacological treatments for knee osteoarthritis includes several classes of medications, each with varying levels of evidence to support their efficacy and safety.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
Oral and topical NSAIDs have been shown to be effective, however, they are associated with gastrointestinal, renal and cardiovascular
risks, which must be considered in long-term use [Beaudart et al, 2020; Bannuru et al, 2015; da Costa et al, 2021; Brophy & Fillingham, 2022; Kolasinski et al, 2020].
- Acetaminophen:
Acetaminophen is commonly used for pain relief in knee OA, its
efficacy is generally lower compared to NSAIDs, but has a favorable safety profile [Bannuru et al, 2015; Brophy & Fillingham, 2022].
- Duloxetine:
Duloxetine, or Cymbalta, is a serotonin-norepinephrine reuptake inhibitor and has been shown to improve pain and function in knee OA [Kolasinski et al, 2020].
- Opioids:
Opioids are generally not recommended due to their
limited efficacy and high risk of adverse effects, including dependency
and overdose [da Costa et al, 2021; Brophy & Fillingham, 2022].
Corticosteroid injections:
Viscosupplementation injections:
Viscosupplementation injections, or intra-articular hyaluronic acid injections, are commonly used for knee pain, and have been approved by the US Food and Drug Administration (FDA) since 1997 [Beaudart et al, 2020; Bannuru et al, 2015; Brophy & Fillingham, 2022].
- Evidence supports the use of intra-articular hyaluronic acid injections for the management of knee osteoarthritis (OA) and repeated hyaluronic acid injections appear to be effective and safe [Altman et al, 2018]:
- A meta-analysis by Wang et al. demonstrated that hyaluronic acid injections significantly improve pain and functional outcomes in knee OA patients, with few adverse events reported [Wang et al, 2004].
- Another meta-analysis by Bannuru et al. highlighted that hyaluronic acid injections show a therapeutic trajectory, with efficacy starting at 4 weeks, peaking at 8 weeks, and maintaining a residual effect up to 24 weeks [Bannuru et al, 2011].
- The American Academy of Orthopaedic Surgeons (AAOS) guidelines indicate that hyaluronic acid injections have a clinically meaningful effect size, although there is some inconsistency in the literature regarding their overall efficacy [Vangsness et al, 2020].
- Maheu et al. emphasized that hyaluronic acid injections offers moderate symptomatic benefits and a good benefit/risk ratio, advocating for its inclusion in knee OA management [Maheu et al, 2019].
Learn more about viscosupplementation injections for knee pain here.
Orthobiologic Injections:
What is the evidence for platelet-rich plasma (PRP) in the treatment of knee osteoarthritis (OA)?
Platelet-rich plasma (PRP) has been studied for knee osteoarthritis (OA) and can be effective in temporarily reducing pain and improving function, with recent studies highlighting the importance of platelet dose:
- A systematic review and meta-analysis by Xiong et al. demonstrated that PRP injections significantly improve pain and functional outcomes in patients with knee OA compared to controls [Xiong et al, 2023].
- Chu et al. conducted a randomized clinical trial comparing PRP to sham saline injections. The study found that PRP provided sustained improvements in clinical outcomes for up to 24 months, with significant differences favoring PRP over saline at all follow-up points [Chu et al, 2022].
- Daiet al. performed a meta-analysis of randomized controlled trials and found that PRP was more effective than hyaluronic acid (HA) and saline in reducing pain and improving function at 6 and 12 months after the PRP injection. The study concluded that PRP provides significant clinical improvements in pain relief and functional outcomes [Dai et al, 2017].
- The American Society of Pain and Neuroscience, in their STEP guidelines, supports the use of PRP for knee OA, highlighting its excellent safety profile and superior efficacy compared to HA in reducing long-term pain and improving knee function [Hunter et al, 2022].
- A systematic review by Berrigan et al. found that higher platelet doses in PRP injections are associated with better clinical outcomes. Specifically, studies with positive outcomes had a mean platelet dose of approximately 5.5 billion platelets, whereas those without significant improvements had lower doses around 2.3 billion platelets [Berrigan et al, 2024]. This suggests that a greater platelet dose may enhance the therapeutic efficacy of PRP in knee OA and the importance of being able to count platelet doses.
- Bansal et al. conducted a study comparing PRP to hyaluronic acid (HA) and found that a PRP dose of 10 billion platelets provided significant improvements in WOMAC and IKDC scores, as well as pain-free walking distance, with benefits persisting up to one year [Bansal et al, 2021]. This study underscores the importance of optimizing the platelet concentration in PRP formulations for sustained clinical efficacy.
- A meta-analysis by Tao et al. demonstrated that multiple doses of PRP are more effective than a single dose in providing pain relief and functional improvement up to one year post-injection [Tao et al, 2023]. This finding supports the use of repeated PRP injections for enhanced outcomes in knee OA.
- What is the evidence for micro-fragmented adipose tissue (MFAT) and bone marrow aspirate concentrate (BMAC) mesenchymal stem cell (MSC) injections in the treatment of knee osteoarthritis? (Learn more about MFAT injections here and BMAC injections here)
- A study by Mautner et al. compared MFAT and BMAC injections in patients with symptomatic knee OA. Both groups showed significant improvements in pain and function. There was no significant difference in outcomes between the two groups, indicating that both MFAT and BMAC are effective for knee OA [Mautner et al, 2019].
- The American Society of Pain and Neuroscience's STEP Guidelines also support the use of MSCs, including those derived from bone marrow and adipose tissue, for knee OA. The guidelines highlight that MSCs improve pain and function, with significant decreases in pain scores. However, the evidence for cartilage repair remains inconclusive [Hunter et al, 2022].
- A systematic review by Keeling et al. found that BMAC injections significantly improved pain and patient-reported outcomes in knee OA patients at short- to mid-term follow-up. However, BMAC did not demonstrate clinical superiority over other biologic therapies, including PRP and MFAT [Keeling et al, 2022].
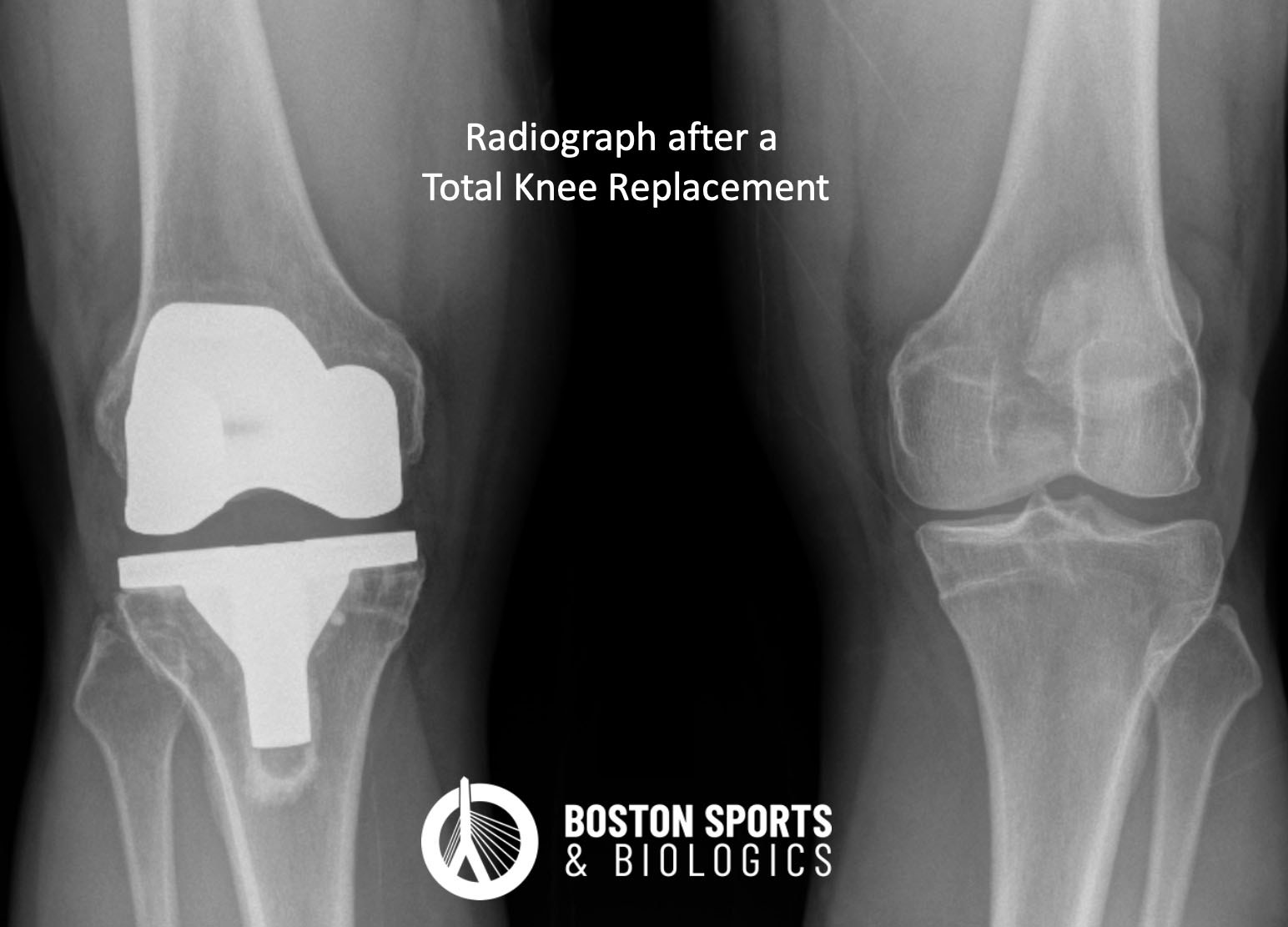
Surgical Management
- The above are potential management tools to help with pain and function, but the definitive treatment for knee arthritis is a joint replacement (total knee replacement).