

A Haglund’s deformity is a bony bump over the back of the heel, and is also known as retrocalcaneal exostosis. This enlargement of the bone is in the back of the heel where the Achilles tendon inserts. Haglund syndrome is when this bony bump causes pain in the overlying Achilles tendon or bursa.
The area of enlarged bone rubs against shoes irritating the soft tissue over the back of the heel. This can cause pain in the bursa that is pressed between the Achilles tendon and the Haglund bump or the Achilles tendon itself.
Symptoms include a noticeable bump on the back of the heel, swelling, redness and inflamed tissue and pain over the back of the heel. Patients often describe pain when walking, especially after a period of rest, or when moving the foot up (dorsiflexion).
Haglund’s deformity is a radiographic finding, and lateral radiographs, or x-rays, are often enough to make a diagnosis of a Haglund’s syndrome.
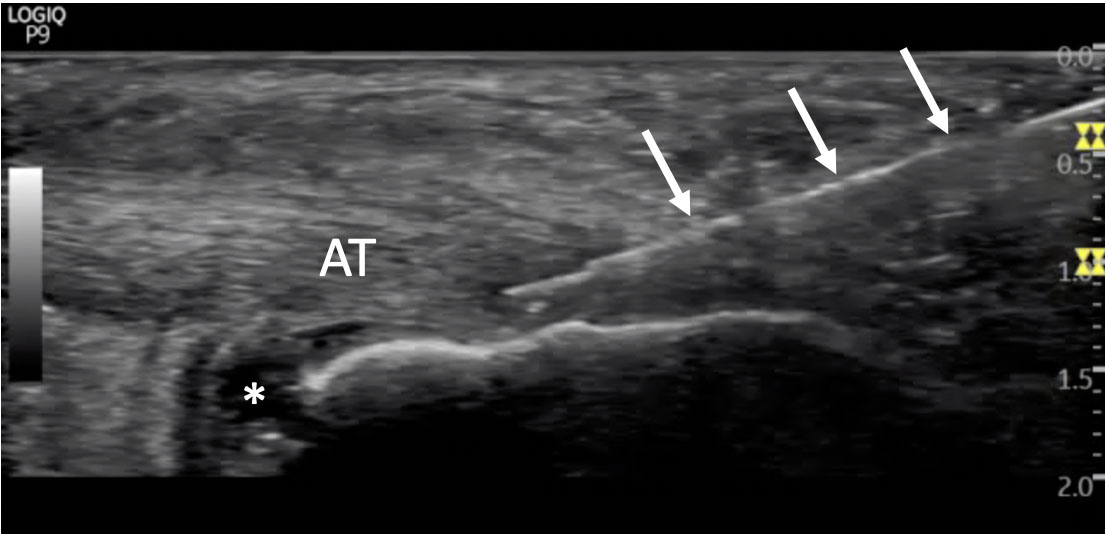
While the bony bump of a Haglund’s deformity predisposes patients to Haglund’s syndrome, this bony bump is not always painful. Haglund deformity irritates the overlying bursa leading. A clinical examination and imaging a diagnostic ultrasound or MRI can rule out associated bursitis or Achilles tendon pathology.
Haglund syndrome and insertional Achilles tendon pain can have overlapping symptoms. It is important to note that Haglund’s syndrome is different from Achilles tendonitis, although both can co-exist.
Haglund’s syndrome is a risk factor for insertional Achilles tenodonitis, but these are two distinct problems. Clearly distinguishing between these two diagnoses will help determine the appropriate treatment. A diagnostic block into the bursa can help confirm the diagnosis of Haglund’s syndrome. This is an in-office procedure using ultrasound guidance. If the pain resolves for a few hours after the injection, this procedure help rule out another diagnosis and confirm the pain is coming from the Haglund's deformity.
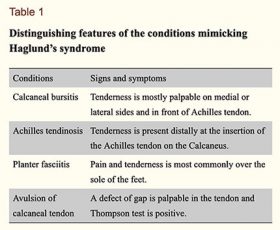
Table 1 used with permission from Haglund’s Syndrome: A Commonly Seen Mysterious Condition 2016, Vaishya et al.
Haglund’s syndrome is often treated conservatively by altering shoe wear, orthotics, physical therapy and anti-inflammatory drugs. Heel pads and wearing open heel shoes can decrease the irritation of the soft tissue over the back of the heel.
In cases that do not respond, surgery can remove the enlarged bone over the heel. Surgical treatments include retrocalcaneal decompression and calcaneal osteotomy to remove the bony bump.
Traditional surgical approaches use general or regional anesthesia, and can be performed with an open incision along the side of the ankle. Patients are usually restricted in a cast for 2 weeks, and not allowed to weight bear on the leg for 2-3 weeks after the procedure. Endoscopic surgical resection may speed recovery.
Swelling can persists for 6 months to a year following surgery, and return to sport may take 6 to 12 months after an open procedure. Endoscopic surgery typically allows for a quicker recovery, but return to sports and running may still take about 12 weeks after surgery (Jerossch & Nasef 2003). Reported surgical complications include Achilles tendon avulsion, persistent heel pain, wound breakdown, nerve injuries and stiffness (Vaishya et al. 2016).
In 2019, Tenex released a TX bone needle that is designed to remove bone. The new needle can replicate the endoscopic Haglund calcaneoplasty.
The procedure is performed in an outpatient surgical setting using only local anesthesia (nerve block). There is a small incision made over the back of the heel. The incision is so small that it requires no sutures.
The specialized TX bone needle is inserted using ultrasound guidance. The cutting action is activated and removes the bony prominence against the Achilles tendon. The procedure typically is completed in less than 10 minutes.
You are allowed to walk in a boot immediately after surgery. You will typically wear the boot when walking for 10 to 21 days depending on how much bone is removed and if there is any damage to the Achilles tendon that needs to be addressed. When the boot is removed you will start working on range of motion exercises, and strengthening. Depending on how the area is healing you can start a progressive return to sports and running between 6 and 12 weeks after the procedure.

The advantages of Tenex over traditional surgery is a shorter recovery time, rapid return to work and sports, no need for general anesthesia, and a small incision with good scar healing.
Platelet-rich plasma (PRP) has become one of the most discussed treatments in sports medicine and orthobiologics. It’s used for knee osteoarthritis, tendinopathy, muscle injury, and more. But despite its growing
Read MoreMeniscus tears are one of the most common causes of knee pain in active adults and aging athletes alike. If you’ve been told you have a “degenerative meniscus tear,” you may have also heard that surgery isn’t always the
Read More