The peroneal nerve runs through the lateral portion of the lower leg, splitting into three branches, the common, superficial and deep nerve.
Entrapment of the peroneal nerve is the most common of lower extremity neuropathies [Fortier et al, 2021].
These nerves are supposed to glide smoothly around surrounding tissue, but entrapped nerves can be stuck or adhered to the surrounding tissue.The most common cause of peroneal nerve entrapment is compression, which can occur due to various factors including prolonged leg crossing, tight casts or braces, trauma, or anatomical variations. Nerves can alsobe compressed by trauma, scar tissue from surgery, or surrounding anatomic structures.
Common peroneal nerve entrapment is when the common peroneal branch of the sciatic nerve is compressed. This nerve is responsible for innervating the muscles that lift the foot and toes, as well as providing sensation to the lateral aspect of the lower leg and the dorsum of the foot. Common peroneal nerve entrapment most commonly occurs at the fibular head.
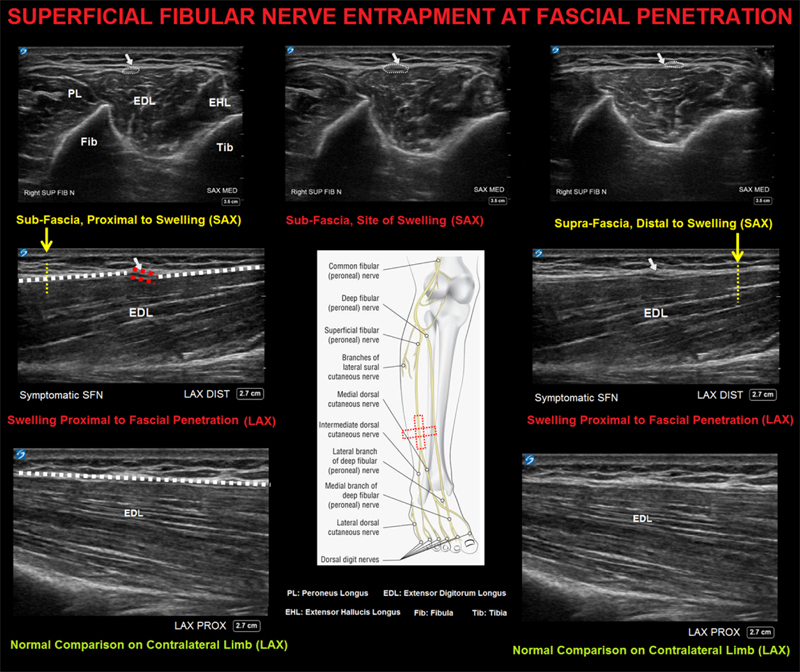
Superficial peroneal nerve entrapment is a condition where the superficial peroneal nerve (SPN) is compressed, typically as it exits the fascia to become subcutaneous. This is a sensory nerve.
Common peroneal nerve entrapment and superficial peroneal nerve entrapment present with distinct clinical symptoms due to the different anatomical locations and functions of the nerves involved.
Common peroneal nerve entrapment typically occurs at the fibular head and presents with [Souter et al, 2018; Poage et al, 2016; Bowley & Doughty, 2019]:
Symptoms can range from mild discomfort to numbness, weakness in the lower leg and foot or foot drop or severe pain.
Diagnosis is based on detailed history, physical examination and imaging. Certain physical tests may be utilized to reproduce symptoms and measure strength and sensation which may vary depending on the location and nerve involved.
Electrodiagnostic Studies: Electrodiagnostic (EDX) studies, including nerve conduction studies (NCS) and electromyography (EMG) are typically used to confirm the diagnosis and localize the site of entrapment. These studies help differentiate peroneal neuropathy from other conditions such as lumbar radiculopathy [Marciniak, 2013; Fabre et al, 1998].
Imaging Techniques: Diagnosti ultrasound and magnetic resonance imaging
(MRI) are valuable adjuncts in the diagnostic workup. Ultrasound is
particularly useful for visualizing superficial nerves and identifying
compressive lesions like ganglion cysts. MRI, including high-resolution
MR neurography, provides detailed evaluation of the nerve's course and
surrounding structures, aiding in the identification causes of entrapment. Studies have shown that both
ultrasound and MRI have high sensitivity and specificity for diagnosing
peroneal nerve entrapment, with some evidence favoring ultrasound for
its diagnostic performance [Oosterbos et al, 2022; Lai et al, 2014; Donovan et al, 2010; Garwood et al, 2018; Luz et al, 2014].
Conservative Management
Initial treatment of pain caused by nerve entrapment consists of rest, ice, NSAIDs, relief of pressure at the site of pain, and stretching exercises [Poage et al, 2016; Klifto et al, 2022; Myers et al, 2015].
Hydrodissection
Surgical Intervention
If pain does not respond to any non-operative conservative interventions, surgical decompression of the affected nerve should be considered. Surgical approaches vary depending on which branch of the personal nerve is entrapped with surgical decompression, or neurolysis of the nerve, and has shown favorable outcomes in terms of pain relief and functional recovery [Poage et al, 2016; Fortier et al, 2021; Corriveau et al, 2018; Fabre et al, 1998].
References
Bowley MP, Doughty CT. Entrapment Neuropathies of the Lower Extremity. Med Clin North Am. 2019 Mar;103(2):371-382.
Daghino W, Pasquali M, Faletti C. Superficial peroneal nerve entrapment in a young athlete: the diagnostic contribution of magnetic resonance imaging. J Foot Ankle Surg. 1997 May-Jun;36(3):170-2.
Donovan A, Rosenberg ZS, Cavalcanti CF. MR imaging of entrapment neuropathies of the lower extremity. Part 2. The knee, leg, ankle, and foot. Radiographics. 2010 Jul-Aug;30(4):1001-19.
Fabre T, Piton C, Andre D, Lasseur E, Durandeau A. Peroneal nerve entrapment. J Bone Joint Surg Am. 1998 Jan;80(1):47-53.
Ferreira-Silva N, Galacho J, Ferreira-Dos-Santos G, Clendenen SR, Hurdle MFB. Ultrasound-guided hydrodissection of the superficial peroneal nerve for chronic neuropathic pain: a war veteran's story. Pain Manag. 2022 Jul;12(5):579-586.
Fortier LM, Markel M, Thomas BG, Sherman WF, Thomas BH, Kaye AD. An Update on Peroneal Nerve Entrapment and Neuropathy. Orthop Rev (Pavia). 2021 Jun 19;13(2):24937.
Garwood ER, Duarte A, Bencardino JT. MR Imaging of Entrapment Neuropathies of the Lower Extremity. Radiol Clin North Am. 2018 Nov;56(6):997-1012.
Klifto KM, Azoury SC, Gurno CF, Card EB, Levin LS, Kovach SJ. Treatment approach to isolated common peroneal nerve palsy by mechanism of injury: Systematic review and meta-analysis of individual participants' data. J Plast Reconstr Aesthet Surg. 2022 Feb;75(2):683-702.
Lai LP, Chen B, Kumar S, Desai R, Mendoza J, Foye PM, Stitik TP. Ganglion cyst at the fibular head causing common peroneal neuropathy diagnosed with ultrasound and electrodiagnostic examination: a case report. Am J Phys Med Rehabil. 2014 Sep;93(9):824-7.
Luz J, Johnson AH, Kohler MJ. Point-of-care ultrasonography in the diagnosis and management of superficial peroneal nerve entrapment: case series. Foot Ankle Int. 2014 Dec;35(12):1362-6.
Marciniak C. Fibular (peroneal) neuropathy: electrodiagnostic features and clinical correlates. Phys Med Rehabil Clin N Am. 2013 Feb;24(1):121-37.
Myers RJ, Murdock EE, Farooqi M, Van Ness G, Crawford DC. A Unique Case of Common Peroneal Nerve Entrapment. Orthopedics. 2015 Jul 1;38(7):e644-6.
Oosterbos C, Decramer T, Rummens S, Weyns F, Dubuisson A, Ceuppens J, Schuind S, Groen J, van Loon J, Rasulic L, Lemmens R, Theys T. Evidence in peroneal nerve entrapment: A scoping review. Eur J Neurol. 2022 Feb;29(2):665-679.
Poage C, Roth C, Scott B. Peroneal Nerve Palsy: Evaluation and Management. J Am Acad Orthop Surg. 2016 Jan;24(1):1-10.
Song B, Marathe A, Chi B, Jayaram P. Hydrodissection as a therapeutic and diagnostic modality in treating peroneal nerve compression. Proc (Bayl Univ Med Cent). 2020 May 5;33(3):465-466.
Souter J, Swong K, McCoyd M, Balasubramanian N, Nielsen M, Prabhu VC. Surgical Results of Common Peroneal Nerve Neuroplasty at Lateral Fibular Neck. World Neurosurg. 2018 Apr;112:e465-e472.
Tong O, Bieri P, Herskovitz S. Nerve entrapments related to muscle herniation. Muscle Nerve. 2019 Oct;60(4):428-433.
Yang LJ, Gala VC, McGillicuddy JE. Superficial peroneal nerve syndrome: an unusual nerve entrapment. Case report. J Neurosurg. 2006 May;104(5):820-3.