Traditionally, pain and tenderness felt over the lateral or outside of the hip pain has been diagnosed as trochanteric "bursitis," but this diagnosis has been challenged by imaging, histological and surgical studies.
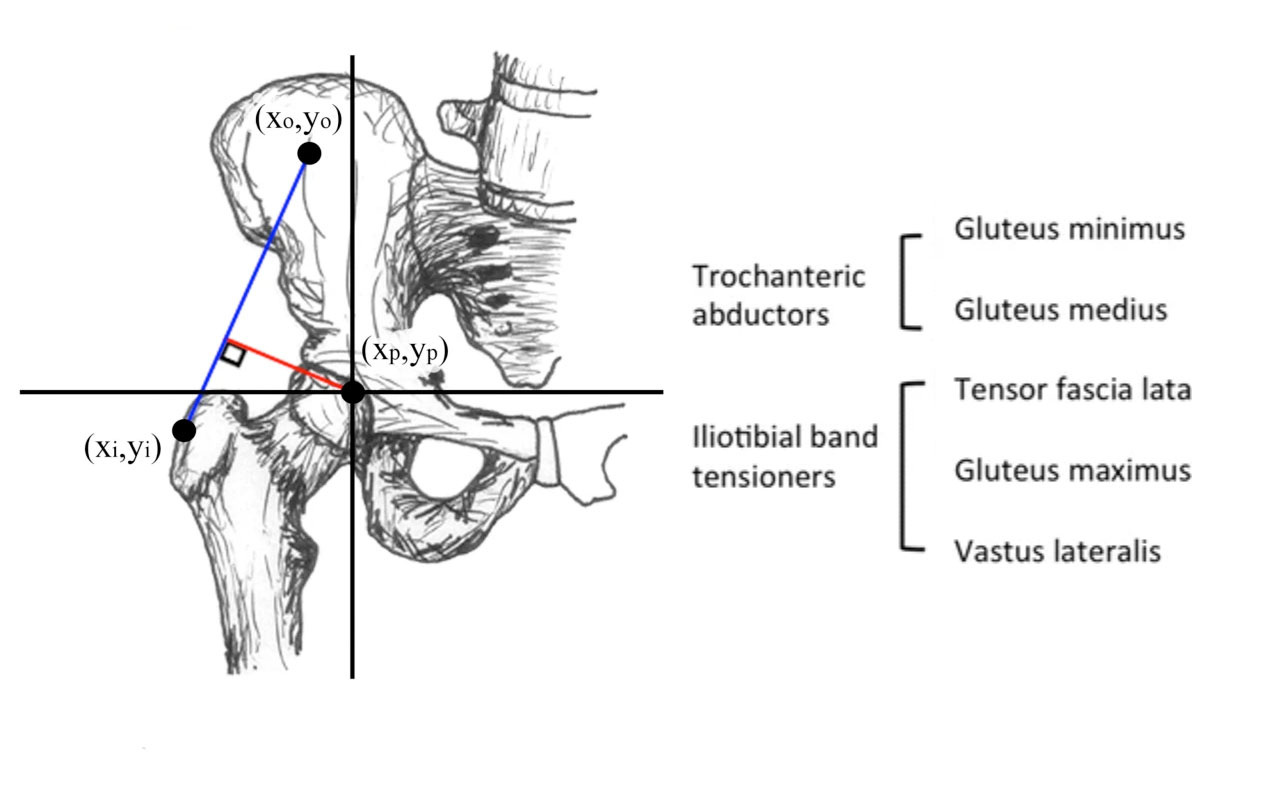
Non-inflammatory tendinopathy of the gluteus medius and/or gluteus minimus is now considered the primary cause of lateral hip pain. Bursal distention may coexist, but this is unlikely to be inflammatory in nature (referring to the suffix “-itis”) [Bird et al, 2001; Blankenbaker et al, 2008; Board et al, 2014; Connell et al, 2003; Fearon et al, 2010; Kingzett-Taylor, 1999; Kong et al, 2007; Pfirrmann et al, 2005; Silva et al, 2008; Walsh, 2006; Wilson et al, 2014].
Gluteal tendinopathy is typically a degenerative process and can involve the gluteus medius or gluteus minimus (Mulligan et al; Reid, 2016; Torres et al, 2018). The condition is sometimes referred to as greater trochanteric pain syndrome to avoid the misnomer or misdiagnosis associated with the historical diagnosis of "hip bursitis."
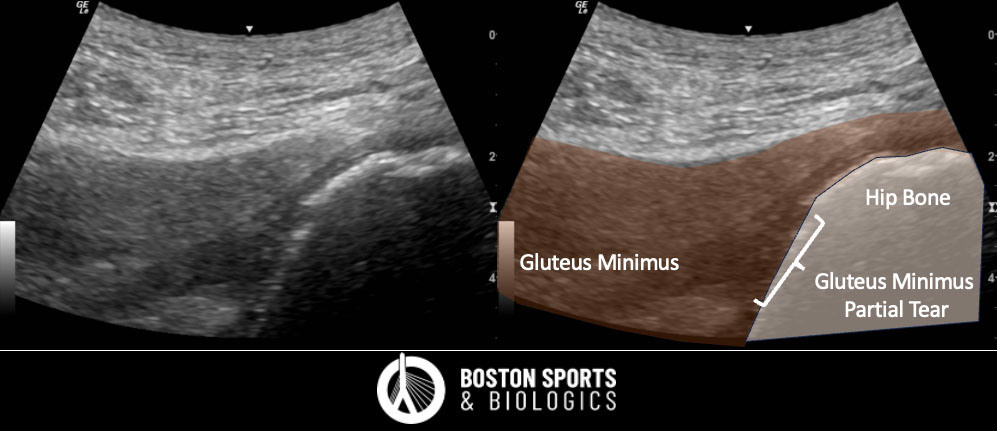
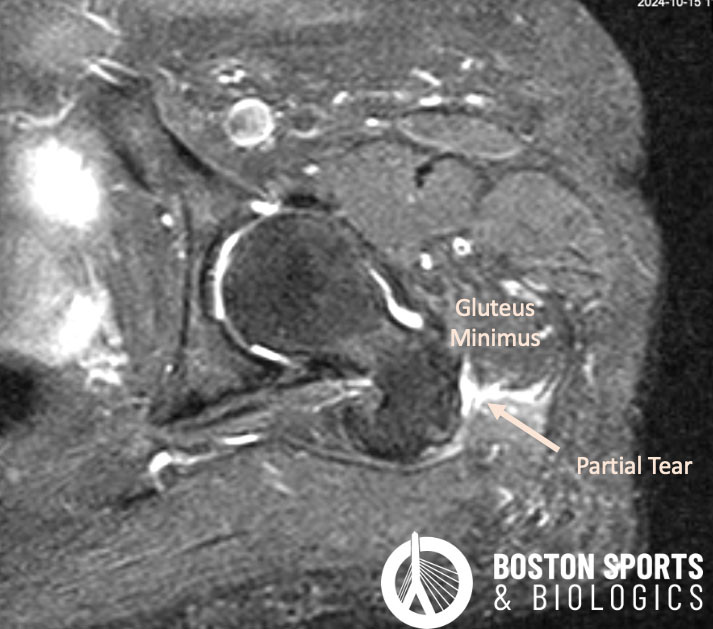
Over time gluteal tendinosis can progress to a partial-thickness tear or full thickness tear of the tendon (Kingzett-Taylor et al; Kong et al).
Patients typically report pain over the lateral hip that worsens with single leg tasks, such as walking, going up stairs or hills, and pain on rising from a seated position or lying on the affected side [Bird et al, 2001; Lequesne, 2006; Strauss et al, 2010; Woodley et al, 2008].
Pain may be felt over the outside of the leg down the thigh or into the buttocks and low back [Lequesne, 2006; Woodley et al, 2008]. Pain can be worse at night.
Diagnosis is based on detailed history,
physical examination, and imaging.
TREATMENT OPTIONS
Different treatment regimens have been described for the management of gluteal tendinopathy, including non-steroidal anti-inflammatory drugs (NSAIDs), physical therapy, shockwave therapy and injections.
Shockwave therapy has been proposed as an alternative treatment for gluteal tendinopathy. Shockwave therapy initiates the
body’s natural healing process with the aim of reduction in pain and
increase in function.
In one randomized trial, when compared to exercise the patients treated with radial shockwave therapy had a superior response (68% had a positive response) at the 4-month follow-up [Rompe et al, 2009]. In a case control study, shockwave therapy was also effective for greater trochanteric pain syndrome [Furia et.al, 2009].
Corticosteroid injections are a potent anti-inflammatory medication and a common treatment for lateral hip pain with good short-term outcomes, but do not provide long-term benefit.
Platelet rich plasma (PRP)
therapy concentrates proteins and growth factors in your own blood, which can promote healing and remodeling of injured tendons. All the following studies reported outcomes of a single ultrasound-guided injection of a non-activated PRP.
In a recent systematic review of 27 studies (1103 patients), the authors reported good evidence for using PRP in the treatment of grade 1 and 2 gluteal tendinopathy. Corticosteroid only showed good outcomes in the short-term (Ladurner et al, 2021).
Percutaneous tendon fenestration or Tenotomy under Ultrasound Guidance are minimally invasive techniques that have been reported to successfully treat gluteal tendinopathy by promoting a bleeding response that stimulates healing without the need for conventional surgery.
In a retrospective study of tendons around the hip and pelvis, 11 patients with gluteal pathology were treated with an ultrasound-guided tendon fenestration procedure using a 20 or 22 gauge spinal needle. Of the patients treated, 11 had tendinosis and 2 had partial tears. The gluteus medius tendon was the most common tendon treated in this study, and 90.9% of patients reported positive outcomes (Jacobson et al, 2015).
In a follow-up study tendon fenestration was compared to PRP in 30 patients with gluteus medius tendinosis. There was no statistically significant difference in outcomes at 3-months with 71% reporting improvement with needle fenestration and 79% reporting improvement with PRP demonstrating similar efficacy for both treatments (Jacobson et al, 2016).
In a case series of 29 patients treated with a tenotomy under ultrasound guidance with the Tenex cutting device for chronic gluteal tendinopathy and/or partial tearing of the gluteus minimus or gluteus medius tendons or both, there was a significant improvement in pain and function. At an average of 22-months, 90% of patients were satisfied and only 10% required surgery (Baker and Mahoney, 2020).
There are also case series reports encouraging results of percutaneous needle tenotomy as a stand-alone treatment for gluteal tendinopathy (Housner et al, 2009).
Surgical management is typically reserved for non-responsive cases. There are a number of surgical approaches that may be used to repair or debride the affected tendon or related structures. Surgical procedures can be divided into: 1) surgical repair of the tendon; and 2) bursectomy and iliotibial band releases.