Patients may experience deep buttock pain with a tendon injury or pain in the back of the thigh with a muscle strain. The pain may worsen with activities such as running, jumping, or prolonged sitting [Sheean et al, 2021].
In acute cases, patients may experience feeling or hearing a “pop” at time of injury. Swelling or bruising around the injured area may also be present.
In some cases the presentation is more insidious and patients can present with a more gradual pain and stiffness in the back of the thigh or buttocks that is worsened with prolonged sitting or running activities.
Diagnosis is based on detailed history, physical examination, and imaging. During the physical examination, a series of provocative tests may be utilized to further determine presence of injury.
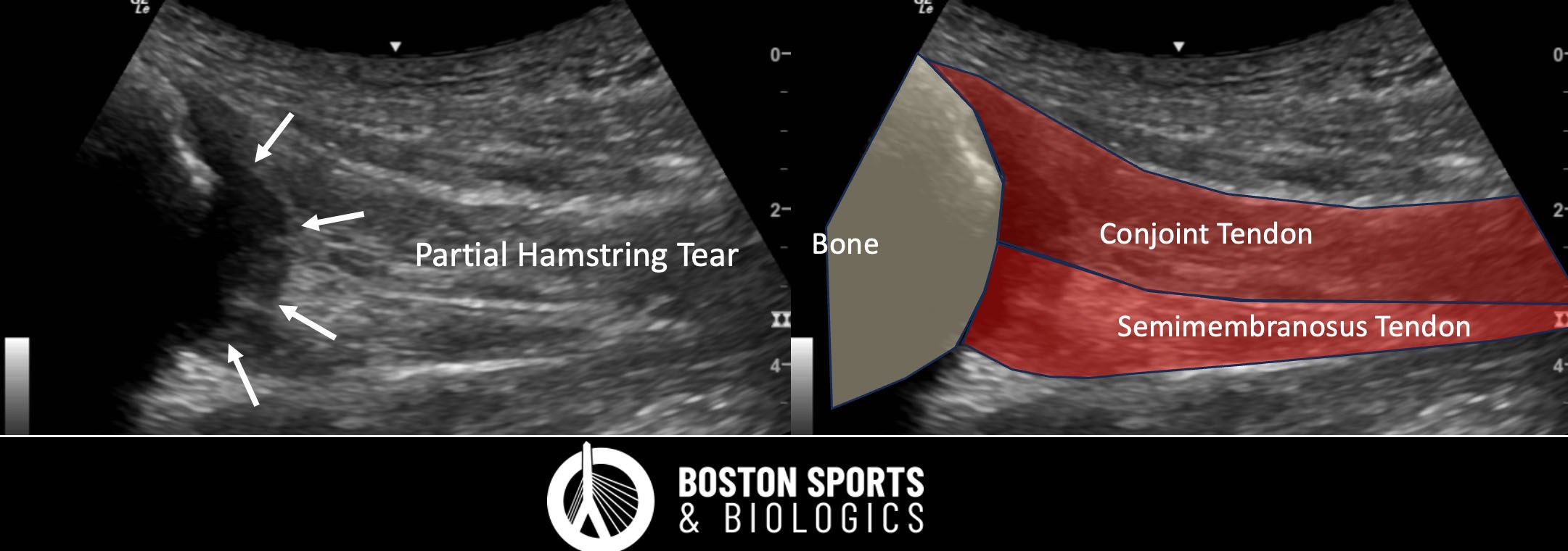
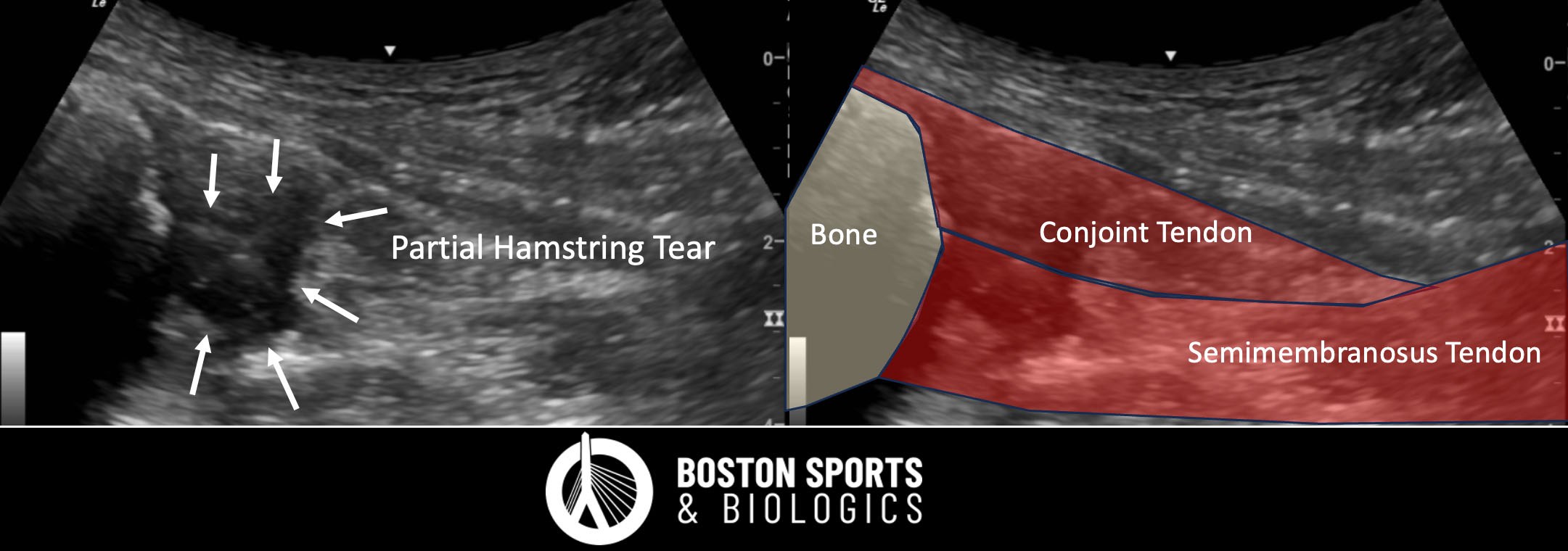
Advanced imaging may be required to confirm diagnosis and determine injury severity. Both magnetic resonance imaging (MRI) and ultrasound effectively identify and assess hamstring injuries, although MRI has been shown to be more accurate than ultrasound for evaluation of deeper muscle injuries [Chu et al, 2017]. An MRI can reveal characteristic changes at the tendon-bone interface [Sheean et al, 2021].
Eccentric strengthening has shown promises in treating tendinopathy, but no randomized controlled trials have specifically looked at eccentric programs for hamstring tendinopathy.
Shockwave therapy may be used as an adjunct therapy for chronic hamstring tendinopathies. Learn more about shockwave therapy here.
Corticosteroid injections for proximal hamstring tendinopathy and hamstring tears have been studied with varying results. Historically, steroids have been used in the treatment of tendon pain, but corticosteroid injections appear to only provide short-term pain relief for proximal hamstring tendinopathy and hamstring tears. The long-term efficacy of corticosteroid injections is questionable, and they may not be the best option for sustained symptom management.
For proximal hamstring tendinopathy:
A study by Zissen et al. demonstrated that ultrasound guided corticosteroid injections provided symptomatic relief in 50% of patients for more than one month, and 24% experienced relief for more than six months suggesting that corticosteroid injections can be effective in the short term for pain relief in tendinopathy [Zissen et al, 2010].
A systematic review by Coombes et al. highlighted that while corticosteroid injections can provide short-term pain relief for tendinopathies, their benefits are not sustained in the intermediate and long term, and they may be associated with worse outcomes compared to other treatments over time [Coombes et al, 2010]. This is consistent with findings in other tendinopathies, suggesting caution in their use for long-term management.
Platelet rich plasma (PRP) is a minimally invasive non-surgical treatment that promotes healing without surgery using a concentration of a patient's own platelets and growth factors injected into the injured area to stimulate healing (learn more about PRP here).
PRP has shown promising results in the literature, specifically in chronic (patients with >3 months of pain) hamstring injuries and appears to offer some benefit in reducing the time to return to play and lowering reinjury rates for partial hamstring tendon tears (Fader et al, 2015).
PRP for chronic hamstring tendon injuries:
Surgical options include debridement and reattachment of the hamstring tendons, particularly in cases of partial or complete tendon avulsions with significant retraction [Sheean et al, 2021; Startzman et al, 2017; Fletcher et al, 2021].
The decision for surgery is guided by the severity of the injury, the degree of tendon retraction, and the patient's functional demands and response to conservative treatment [Allahabadi et al, 2024; Sheean et al, 2021; Fletcher et al, 2021; Plastow et al, 2023; Kayani et al, 2020; Moatshe et al, 2016]. Patients most likely to benefit from surgical interventions for hamstring tendonitis are:
Patients with significant tendon retraction: Specifically, those with proximal hamstring injuries involving two or more tendons with greater than 2 cm of retraction.
Patients with significant tendon retraction: Specifically, those with proximal hamstring injuries involving two or more tendons with greater than 2 cm of retraction.
Patients with symptomatic displaced bony avulsions: These cases often require surgical intervention to restore function and alleviate symptoms.
Surgical intervention for acute complete tendon rupture have shown good to excellent results, and generally results in better functional outcomes, higher rates of return to sport, and greater patient satisfaction compared to nonoperative management [Lefevre et al, 2024; Harris et al, 2011]. Risks of surgery include, infection, nerve damage due to the proximity of the sciatic nerve, deep vein thrombosis (DVT), wound-related complications and prolonged rehabilitation [Fletcher et al, 2021; Devitt, 2018].
In cases of proximal hamstring tendinopathy, surgical treatment may become an option for patients with chronic symptoms that do not respond to conservative treatment [Costa et al, 2016], but for tendinopathy some studies have shown greater pain after the surgery than before [Aldridge et al, 2012].
Learn more about how surgery compares to platelet rich plasma (PRP) here.