Meniscus tears are one of the most common causes of knee pain in active adults and aging athletes alike. If you’ve been told you have a “degenerative meniscus tear,” you may have also heard that surgery isn’t always the best option—and that’s increasingly supported by medical research, with outcomes after arthroscopic partial meniscectomy shown to be no better than those after a sham surgical procedure (Sihvonen et al, 2013).
In recent years, intra-meniscal biologic injections, particularly platelet-rich plasma (PRP), have emerged as a promising non-surgical treatment aimed at reducing pain, improving function, and potentially delaying or avoiding surgery. A 2024 systematic review published in the Journal of Orthopaedics provides the most comprehensive summary to date of how PRP performs for degenerative meniscus tears (Elphingstone et al, 2024).
This article explains what intra-meniscal biologic injections are, how they work, who may benefit most, and what the current evidence actually shows—without hype or exaggeration.
The meniscus is a crescent-shaped cartilage structure that helps absorb shock and distribute load in the knee. Over time, repetitive stress, reduced blood supply, and age-related tissue changes can lead to degenerative meniscus tears, even without a specific injury.
Unlike traumatic tears in young athletes, degenerative tears:
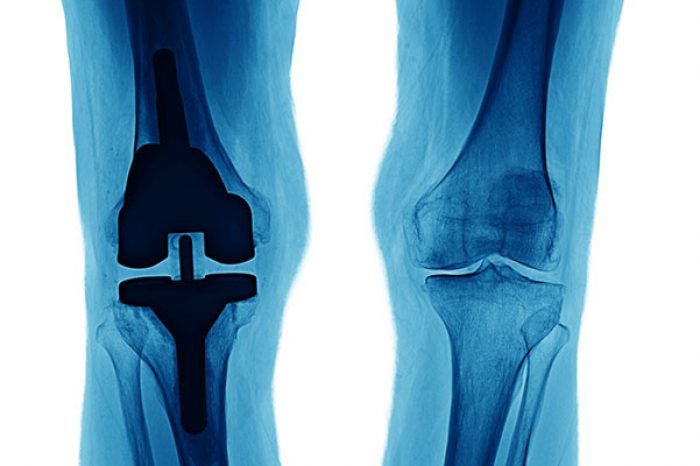
Importantly, large studies have shown that arthroscopic surgery for degenerative meniscus tears often provides little long-term benefit and may accelerate knee osteoarthritis. Research for nearly two decades has consistently shown that arthroscopic meniscus surgery may accelerate knee degeneration rather than prevent it.
This has shifted treatment strategies toward non-operative and biologic approaches.
Platelet-rich plasma (PRP) is created from a small sample of your own blood. After centrifugation, the plasma portion contains a higher concentration of platelets, which release growth factors involved in tissue repair and inflammation modulation.
PRP can be delivered in several ways:
Laboratory and animal studies provide a biologic rationale for PRP use in meniscal pathology. PRP has been shown to:
In simpler terms, PRP may help shift the meniscus from a degenerative, inflammatory state toward a more reparative one .
The 2024 systematic review by Elphingstone et al. analyzed 10 human clinical studies involving 686 patients treated non-operatively with PRP for degenerative meniscus tears .
Key Findings at a Glance
Across multiple studies:
Pain Relief and Function
Patients treated with PRP consistently reported:
Some studies showed benefits lasting up to 2–3 years, especially when multiple PRP injections were used.
One important insight from the Elphingstone et al. review is that how PRP is delivered matters.
Studies using combined intra-articular + intra-meniscal injections showed some of the most durable improvements, suggesting a complementary effect .
Intra-meniscal biologic injections may be most effective for patients who:
Patients with advanced arthritis, large displaced tears, or mechanical locking may still require surgical evaluation.
Across all studies reviewed:
Ultrasound guidance improves injection accuracy and safety, particularly for intra-meniscal delivery.
Boyd JA, Gradisar IM. Total Knee Arthroplasty After Knee Arthroscopy in Patients Older Than 50 Years. Orthopedics. 2016 Nov 1;39(6):e1041-e1044.
Collins JE, Shrestha S, Losina E, Marx RG, Guermazi A, Jarraya M, Jones MH, Levy BA, Mandl LA, Williams EE, Wright RW, Spindler KP, Katz JN; METEOR Investigator Group. Five-Year Structural Changes in the Knee Among Patients With Meniscal Tear and Osteoarthritis: Data From a Randomized Controlled Trial of Arthroscopic Partial Meniscectomy Versus Physical Therapy. Arthritis Rheumatol. 2022 Aug;74(8):1333-1342.
Elphingstone JW, Alston ET, Colorado BS. Platelet-rich plasma for nonoperative management of degenerative meniscal tears: A systematic review. J Orthop. 2024 Mar 12;54:67-75.
Freymann U, Metzlaff S, Krüger JP, Hirsh G, Endres M, Petersen W, Kaps C. Effect of Human Serum and 2 Different Types of Platelet Concentrates on Human Meniscus Cell Migration, Proliferation, and Matrix Formation. Arthroscopy. 2016 Jun;32(6):1106-16.
Hagmeijer MH, Korpershoek JV, Crispim JF, Chen LT, Jonkheijm P, Krych AJ, Saris DBF, Vonk LA. The regenerative effect of different growth factors and platelet lysate on meniscus cells and mesenchymal stromal cells and proof of concept with a functionalized meniscus implant. J Tissue Eng Regen Med. 2021 Jul;15(7):648-659.
Howard D, Shepherd JH, Kew SJ, Hernandez P, Ghose S, Wardale JA, Rushton N. Release of growth factors from a reinforced collagen GAG matrix supplemented with platelet rich plasma: Influence on cultured human meniscal cells. J Orthop Res. 2014 Feb;32(2):273-8.
Hunter CW, Deer TR, Jones MR, Chang Chien GC, D'Souza RS, Davis T, Eldon ER, Esposito MF, Goree JH, Hewan-Lowe L, Maloney JA, Mazzola AJ, Michels JS, Layno-Moses A, Patel S, Tari J, Weisbein JS, Goulding KA, Chhabra A, Hassebrock J, Wie C, Beall D, Sayed D, Strand N. Consensus Guidelines on Interventional Therapies for Knee Pain (STEP Guidelines) from the American Society of Pain and Neuroscience. J Pain Res. 2022 Sep 8;15:2683-2745.
Rongen JJ, Rovers MM, van Tienen TG, Buma P, Hannink G. Increased risk for knee replacement surgery after arthroscopic surgery for degenerative meniscal tears: a multi-center longitudinal observational study using data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2017 Jan;25(1):23-29.
Sihvonen R, Paavola M, Malmivaara A, Itälä A, Joukainen A, Nurmi H, Kalske J, Järvinen TL; Finnish Degenerative Meniscal Lesion Study (FIDELITY) Group. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013 Dec 26;369(26):2515-24.
Qi Y, Tang R, Shi Z, Feng G, Zhang W. Wnt5a/Platelet-rich plasma synergistically inhibits IL-1β-induced inflammatory activity through NF-κB signaling pathway and prevents cartilage damage and promotes meniscus regeneration. J Tissue Eng Regen Med. 2021 Jul;15(7):612-624.
Wang CC, Lee CH, Peng YJ, Salter DM, Lee HS. Platelet-Rich Plasma Attenuates 30-kDa Fibronectin Fragment-Induced Chemokine and Matrix Metalloproteinase Expression by Meniscocytes and Articular Chondrocytes. Am J Sports Med. 2015 Oct;43(10):2481-9.
Wong CC, Kuo TF, Yang TL, Tsuang YH, Lin MF, Chang CH, Lin YH, Chan WP. Platelet-Rich Fibrin Facilitates Rabbit Meniscal Repair by Promoting Meniscocytes Proliferation, Migration, and Extracellular Matrix Synthesis. Int J Mol Sci. 2017 Aug 7;18(8):1722.
Xu H, Zou X, Xia P, Aboudi MAK, Chen R, Huang H. Differential Effects of Platelets Selectively Activated by Protease-Activated Receptors on Meniscal Cells. Am J Sports Med. 2020 Jan;48(1):197-209.
Platelet-rich plasma (PRP) has become one of the most discussed treatments in sports medicine and orthobiologics. It’s used for knee osteoarthritis, tendinopathy, muscle injury, and more. But despite its growing
Read MoreMeniscus tears are one of the most common causes of knee pain in active adults and aging athletes alike. If you’ve been told you have a “degenerative meniscus tear,” you may have also heard that surgery isn’t always the
Read More