Greater Trochanteric Pain Syndrome (GTPS) is a frustrating causes of chronic hip pain—especially for women and middle-aged adults. Often misdiagnosed and challenging to treat, GTPS affects mobility, daily comfort, and quality of life.
That’s exactly what researchers set out to discover in a systematic literature review on Platelet-Rich Plasma (PRP) therapy for GTPS—and the results are giving new hope to patients and clinicians alike.
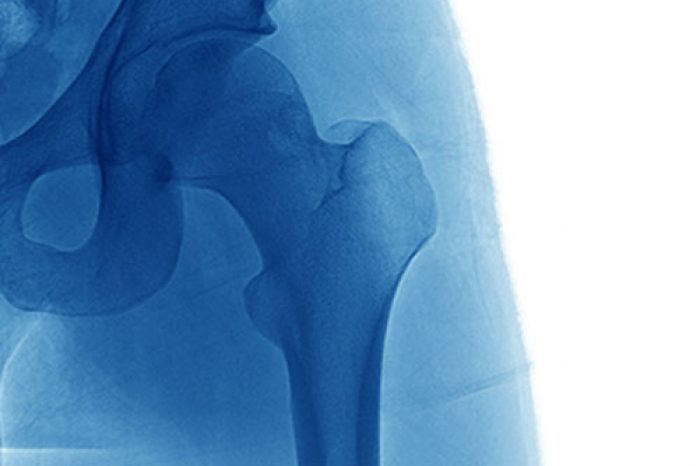
GTPS, sometimes called trochanteric bursitis, refers to pain over the outer part of the hip. It’s often caused not by inflammation of the bursa (as once believed), but by gluteal tendinopathy—chronic wear-and-tear of the gluteus medius and minimus tendons [Long et al, 2013; Grimaldi et al, 2015].
GTPS is common, particularly in middle-aged women, runners, and individuals with low back or knee issues. And while most cases improve with physical therapy and anti-inflammatory medications, chronic GTPS can be stubborn, requiring more advanced treatments like corticosteroid injections, shockwave therapy—or now, PRP [Long et al, 2013; Grimaldi et al, 2015].
The condition is often misdiagnosed as bursitis, but imaging studies, such as ultrasound and MRI, have shown that gluteal tendinopathy is the primary pathology in most cases [Kong et al, 2007; Long et al, 2013].
Platelet-Rich Plasma (PRP) is a regenerative therapy made from a small sample of your own blood. After spinning it in a centrifuge to concentrate the platelets, the resulting solution is injected into the damaged tissue.
Why platelets? They’re packed with growth factors—which are essential for the healing process [Sheean et al, 2021; Dos Santos et al, 2021].
These factors promote cellular proliferation, migration, and differentiation, which are critical for tissue regeneration. For instance, PRP has been shown to enhance the healing of tendons, ligaments, and muscles by increasing collagen production, cellularity, and vascularity [Chalidis et al, 2023; Etulain, 2018].
PRP has already shown promise for:
The review by Ali et al., published in the Journal of Hip Preservation Surgery, analyzed nine studies on PRP for GTPS, including:
In total, 209 patients were studied—mostly women, with a mean age of 58—and all had symptoms lasting longer than 3 months.
YES, This systematic review shows most studies report reduced pain, improved function, and longer-lasting benefits compared to corticosteroids.
The research still lacks:
Corticosteroid injections are commonly used for short-term relief of GTPS, but:
While they often provide quick pain relief, multiple studies show no long term benefit. PRP, on the other hand, aims to repair the tissue—not just mask the pain.
You may be a candidate for PRP if:
PRP for Greater Trochanteric Pain Syndrome appears to be safe, minimally invasive, and backed by early clinical success. While not yet a universal standard, it offers a viable option for patients who’ve exhausted other treatments.
If you’ve been struggling with GTPS and haven’t found lasting relief, PRP could be worth exploring. Learn more at:
(781) 591-7855
20 Walnut St
Suite 14
Wellesley MA 02481
Meniscus tears are one of the most common causes of knee pain in active adults and aging athletes alike. If you’ve been told you have a “degenerative meniscus tear,” you may have also heard that surgery isn’t always the
Read MoreFor patients with chronic adductor longus tendinopathy, a newer option is emerging: ultrasound-guided tenotomy using the Tenex system. Recent clinical evidence suggests this minimally invasive approach may effectively
Read More